Oncocytic Neoplasm on Renal Mass Biopsy: A Diagnostic Conundrum
A 56-year-old man presented with a 4.5-cm leftsided renal mass incidentally discovered on an ultrasound performed for workup of lupus nephritis. On dedicated contrast-enhanced magnetic resonance imaging (MRI), the tumor was found to be avidly enhancing.
Oncology (Williston Park). 30(5):426–428, 435.

Figure 1. Axial MRI Images of the Patient’s 4.5-cm Renal Tumor
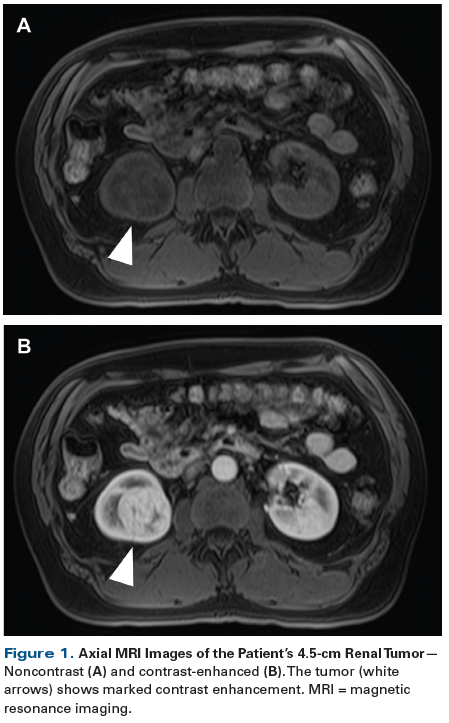
Figure 2. Hematoxylin and Eosin–Stained Sections of the Patient’s Renal Mass Biopsy
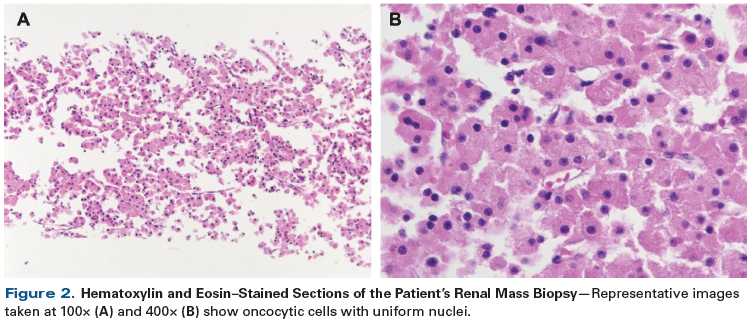
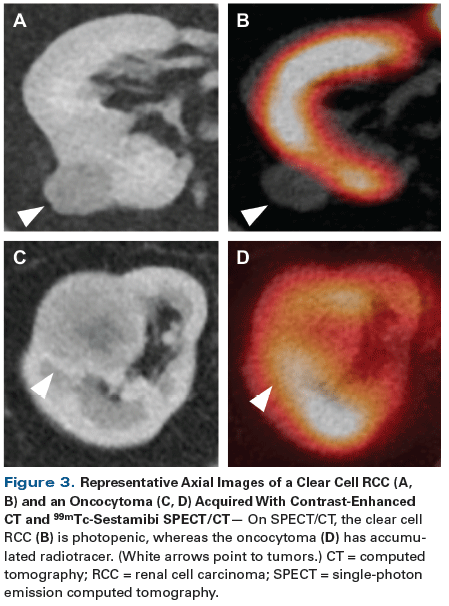
Figure 3. Representative Axial Images of a Clear Cell RCC (A, B) and an Oncocytoma (C, D) Acquired With Contrast-Enhanced CT and 99mTc-Sestamibi SPECT/CT
The Case
A 56-year-old man presented with a 4.5-cm leftsided renal mass incidentally discovered on an ultrasound performed for workup of lupus nephritis. On dedicated contrast-enhanced magnetic resonance imaging (MRI), the tumor was found to be avidly enhancing (Figure 1). In light of the patient’s history of lupus nephritis and related concerns over future declines in renal function, the patient elected to undergo renal mass biopsy prior to deciding on the mode of treatment. A core needle biopsy was performed and pathologic review of the specimen demonstrated an oncocytic renal neoplasm (Figure 2).
Which of the following represents the best next step in management of this patient?
A. Additional imaging with contrast-enhanced computed tomography (CT).
B. Repeat biopsy.
C. Ultrastructural evaluation of the tissue with electron microscopy.
D. Evaluation of the tissue with immunohistochemical staining.
E. Shared decision making, offering the patient a choice of active surveillance vs intervention.
Discussion
In recent decades, the frequency of incidentally detected renal tumors has risen substantially.[1-3] This, in turn, has led to the overtreatment of increasing numbers of benign and indolent renal tumors.[2,4] In an effort to curtail this trend, many have advocated for a risk-adapted approach when faced with a patient presenting with an incidental renal mass.[5-7] At the core of such an approach is assessment of the histology of the tumor. Common renal tumor histologies include benign entities, such as oncocytomas and angiomyolipomas, as well as the clear cell, papillary, and chromophobe subtypes of renal cell carcinoma (RCC).[8] In general, clear cell and type II papillary RCCs are considered to be aggressive, whereas type I papillary and chromophobe RCCs are more indolent in nature. Because anatomic imaging techniques are unable to reliably differentiate between the various renal tumor histologies (making Answer A incorrect), this task is most often performed via renal mass biopsy. According to a recent systematic review, this procedure can be safely performed with a diagnostic yield in approximately 90% of cases.[9]
The goal of renal mass biopsy is to determine the precise histology of a given tumor. While this is possible in the majority of cases, it is not uncommon for the interpreting pathologist to use the catchall term of “oncocytic renal neoplasm” to describe a tumor in which the constituent cells contain pink or eosinophilic cytoplasm. In one reported series on renal mass biopsy, this diagnosis of “oncocytic renal neoplasm” was provided in 11.5% of cases.[10] The reason for the use of this inexact descriptor is the fact that a number of renal tumor histologies can contain oncocytic components (albeit in varying amounts), making them difficult to distinguish on renal mass biopsy.[11-13] These histologies include oncocytoma, hybrid oncocytic/chromophobe tumors (HOCTs), the eosinophilic variant of chromophobe RCC, papillary RCC, clear cell RCC with predominantly eosinophilic features, and unclassified RCC.
Because of the varying malignant potential of tumors that fall within the category of “oncocytic renal neoplasm,” receiving this diagnosis presents a conundrum for the treating physician. If the urologist were confident that the diagnosis was an oncocytoma or HOCT, active surveillance would likely be pursued. In contrast, knowledge that the patient was harboring a more aggressive tumor type would likely lead to an intervention with surgery or thermal ablation. Unfortunately, little can be done to resolve the histologic diagnosis with use of repeat biopsy (Answer B) or ancillary evaluation of the tissue. More specifically, although electron microscopy[11] (Answer C) and immunohistochemistry for markers such as cytokeratin 7 and S100A1[12,13] (Answer D) have been proposed to aid in refining the diagnosis, these techniques cannot often be practically performed with the limited amount of tissue obtained on a core needle biopsy. Moreover, these tests offer only limited diagnostic accuracy.[10,12,13] Thus, the physician and patient are left to base the decision to intervene on the model of shared decision making, incorporating factors such as patient age, life expectancy, preoperative renal function, risk of perioperative morbidity, and overall patient preference (Answer E).
KEY POINTS
- Percutaneous biopsy is a relatively safe and accurate method for determining the histology of renal tumors. This diagnostic procedure is increasingly being performed to risk-stratify patients presenting with an incidentally detected renal tumor.
- Approximately 10% of biopsied renal masses will be classified as an “oncocytic renal neoplasm.” Although the majority of these lesions will be benign oncocytomas, a handful of malignant renal tumor types can contain oncocytic cells, leaving some uncertainty regarding the exact histologic diagnosis.
As an adjunct to evaluating patients with an oncocytic neoplasm on renal mass biopsy, our group has pioneered the use of 99mTc-sestamibi single-photon emission computed tomography/computed tomography (SPECT/CT) for imaging clinically localized renal tumors.[14,15] 99mTc-sestamibi is a lipophilic cation that preferentially accumulates in tumors with a high density of mitochondria, such as benign renal oncocytomas and HOCTs (Figure 3). In a recently published prospective study, we found that 99mTc-sestamibi SPECT/CT correctly identified 5 of 6 oncocytomas (83.3%) and 2 of 2 HOCTs (100%), resulting in an overall sensitivity of 87.5%.[15] Notably, only 2 of 42 tumors of other histoloties were falsely positive on SPECT/CT (both were small eosinophilic chromophobe RCCs), resulting in a specificity of 95.2%. Additionally, in our expanded experience with this test, we have seen no false-positive oncocytic neoplasm with a high malignant potential, such as a type II papillary RCC, clear cell RCC, or unclassified RCC. Thus, we believe that, with further validation, this test has the potential to help urologists overcome the conundrum of the oncocytic renal neoplasm on needle biopsy.
Outcome of This Case
Although highest on the differential diagnosis for this patient’s renal mass was an oncocytoma, due to concern for a possible RCC, the patient elected to undergo treatment with a robotic-assisted laparoscopic partial nephrectomy. The surgery was completed without complication, and on final surgical pathology, the patient was found to have a benign oncocytoma. The patient is currently doing well; however, as a result of the surgery, he has experienced a decline in his estimated glomerular filtration rate from 80 mL/min/1.73m2 to a new baseline of 65 mL/min/1.73m2.
Financial Disclosure: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
E. David Crawford, MD, serves as Series Editor for Clinical Quandaries. Dr. Crawford is Professor of Surgery, Urology, and Radiation Oncology, and Head of the Section of Urologic Oncology at the University of Colorado School of Medicine; Chairman of the Prostate Conditions Education Council; and a member of ONCOLOGY's Editorial Board.
If you have a case that you feel has particular educational value, illustrating important points in diagnosis or treatment, you may send the concept to Dr. Crawford at david.crawford@ucdenver.edu for consideration for a future installment of Clinical Quandaries.
References:
1. Cooperberg MR, Mallin K, Ritchey J, et al. Decreasing size at diagnosis of stage 1 renal cell carcinoma: analysis from the National Cancer Data Base, 1993 to 2004. J Urol. 2008;179:2131-5.
2. Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK. Rising incidence of small renal masses: a need to reassess treatment effect. J Natl Cancer Inst. 2006;98:1331-4.
3. Laguna MP, Algaba F, Cadeddu J, et al. Current patterns of presentation and treatment of renal masses: a clinical research office of the Endourological Society prospective study. J Endourol. 2014;28:861-70.
4. Johnson DC, Vukina J, Smith AB, et al. Preoperatively misclassified, surgically removed benign renal masses: a systematic review of surgical series and United States population level burden estimate. J Urol. 2015;193:30-5.
5. Halverson SJ, Kunju LP, Bhalla R, et al. Accuracy of determining small renal mass management with risk stratified biopsies: confirmation by final pathology. J Urol. 2013;189:441-6.
6. Blute ML Jr, Drewry A, Abel EJ. Percutaneous biopsy for risk stratification of renal masses. Ther Adv Urol. 2015;7:265-74.
7. Gorin MA, Rowe SP, Allaf ME. Nuclear imaging of renal tumours: a step towards improved risk stratification. Nat Rev Urol. 2015;12:445-50.
8. Srigley JR, Delahunt B, Eble JN, et al. The International Society of Urological Pathology (ISUP) Vancouver classification of renal neoplasia. Am J Surg Pathol. 2013;37:1469-89.
9. Marconi L, Dabestani S, Lam TB, et al. Systematic review and meta-analysis of diagnostic accuracy of percutaneous renal tumour biopsy. Eur Urol. 2016;69:660-73.
10. Leveridge MJ, Finelli A, Kachura JR, et al. Outcomes of small renal mass needle core biopsy, nondiagnostic percutaneous biopsy, and the role of repeat biopsy. Eur Urol. 2011;60:578-84.
11. Johnson NB, Johnson MM, Selig MK, Nielsen GP. Use of electron microscopy in core biopsy diagnosis of oncocytic renal tumors. Ultrastruct Pathol. 2010;34:189-94.
12. Kryvenko ON, Jorda M, Argani P, Epstein JI. Diagnostic approach to eosinophilic renal neoplasms. Arch Pathol Lab Med. 2014;138:1531-41.
13. Khor LY, Tan PH. Diagnostic biomarkers in eosinophilic renal neoplasms. Urol Clin North Am. 2016;43:87-94.
14. Rowe SP, Gorin MA, Gordetsky J, et al. Initial experience using 99mTc-MIBI SPECT/CT for the differentiation of oncocytoma from renal cell carcinoma. Clin Nucl Med. 2015;40:309-13.
15. Gorin MA, Rowe SP, Baras AS, et al. Prospective evaluation of 99mTc-sestamibi SPECT/CT for the diagnosis of renal oncocytomas and hybrid oncocytic/chromophobe tumors. Eur Urol. 2016;69:413-6.