Oral Metabolism Drug Active in Acute Myeloid Leukemia
New trial results show that a novel, oral metabolic inhibitor has demonstrated early activity in relapsed or refractory acute myeloid leukemia (AML), according to data presented at the annual meeting of the American Association of Cancer Research.
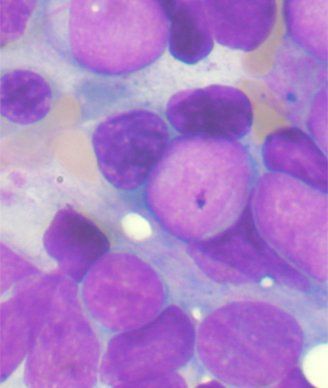
Bone marrow aspirate showing AML; source: Tontoni, Wikimedia Commons
Results presented at the annual meeting of the American Association of Cancer Research show that a novel, oral metabolic inhibitor (AG-221) has demonstrated early activity in relapsed or refractory acute myeloid leukemia (AML), a particularly difficult to treat hematological malignancy.
AG-221 was administered to patients on the trial at twice-daily doses of 30 mg, 50 mg, 75 mg, and 100 mg. Patients had a median of two prior therapies.
Complete remissions were seen at the 30 mg and 50 mg doses.
Six of the 10 patients that could be evaluated for efficacy had an objective response. Five of these patients were treated with 30 mg and five were treated with 50 mg.
One patient in the 30 mg cohort and two patients in the 50 mg cohort had complete responses. Two patients, one in each of these cohorts, had a complete response with incomplete platelet recovery. One patient in the 50 mg cohort had a partial response.
Fourteen of the 19 patients remain on treatment.
Responses were fairly rapid, occurring late in cycle 3 or early cycle 4 in the 30 mg cohort and by cycle 3 at the latest in the 50 mg cohort, said Eytan M. Stein, MD, physician at Memorial Sloan-Kettering Cancer Center in New York who specializes in acute and chronic leukemia treatment, during a press briefing.
“This is an extremely exciting result,” said Stein at the briefing, noting that the data is still early and needs longer follow-up. “This kind of data is unheard of in a relapsed, refractory AML setting where survival is typically less than 10%,” he added.
The drug, AG-221, a first-in-class inhibitor of isocitrate dehydrogenase 2 (IDH2)-mutant metabolic enzyme was also well tolerated in 21 refractory AML patients and 1 myelodysplastic syndrome (MDS) patient.
All patients enrolled on the study were IDH2-mutant positive.
Thus far, therapy has been well tolerated with no dose-limiting toxicities reported and a no maximum tolerated dose reached. Two potential drug-related severe adverse events, grade 2 hyperleukocytosis and grade 3 confusion, were observed in two patients. In the first patient cohort (30 mg), three patients died of sepsis within 30 days of stopping treatment. One of these could be related to the drug treatment.
IDH2 mutations have been identified in both solid tumors and hematological malignancies including glioblastoma, AML, and MDS. Approximately 10% to 15% of AML patients harbor an IDH2 mutation.
“Mutations in the genes for the metabolic enzymes IDH1 and IDH2 are thought to be the drivers of distinct subsets of acute myeloid leukemias,” said Stein. “They lead to the production of increased levels of an oncometabolite called 2-hydroxyglutarate (2-HG), which is hypothesized to prevent normal healthy bone marrow cells from maturing, leading to cancer.”
In preclinical studies, accumulation of 2-HG has been shown to inhibit certain epigenetic cell states that can change cell differentiation. Researchers hypothesized that blocking 2-HG could facilitate the continued differentiation of myeloid precursor cells and reverse the AML phenotype.
Pharmacodynamic response on the phase I trial showed a reduction in 2-HG plasma levels as much as 97% after AG-221 dosing.
Dose escalation of AG-221 continues and expansion cohorts are currently being planned to begin in 2014.
Reference
Stein E, Tallman M, Pollyea DA, et al. “Clinical safety and activity in a phase I trial of AG-221, a first in class, potent inhibitor of the IDH2-mutant protein, in patients with IDH2 mutant positive advanced hematologic malignancies.” American Association for Cancer Research Annual Meeting 2014; April 5–9, 2014; San Diego. Abstr CT103.