Orteronel Delays Disease Progression in Advanced Prostate Cancer
The investigational therapy orteronel delayed disease progression in patients with metastatic castration-resistant prostate cancer, but did not significantly improve overall survival.
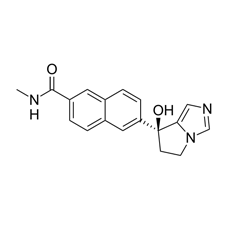
Chemical structure of orteronel
Orteronel, an investigational oral therapy for prostate cancer, improved progression-free survival, but did not significantly improve overall survival in patients with chemotherapy-naive metastatic castration-resistant prostate cancer (mCRPC). The median overall survival of patients treated with orteronel plus the corticosteroid prednisone was 31.4 months compared with 29.5 months for patients treated with prednisone alone (hazard ratio [HR] = 0.9, P = .314).
The median radiographic progression-free survival (rPFS) was 13.8 months compared with 8.7 months in the prednisone-alone arm (HR = 0.7, P < .00001).
The results (abstract #5008) were presented by Ronald de Wit, MD, PhD, of the Erasmus MC Cancer Institute in the Netherlands, at the American Society of Clinical Oncology (ASCO) Annual Meeting, held May 30–June 3, in Chicago.
The ELM-PC 4 phase III international trial randomized 1,560 prostate cancer patients to either 400 mg of orteronel plus 5 mg of prednisone twice daily or placebo plus prednisone.
A higher proportion of patients had a greater than 50% decrease in prostate-specific antigen (PSA) levels in the orteronel treatment arm compared with the control arm (43% vs 25%, P < .00001). Patients treated with orteronel also had favorable circulating tumor cell counts compared with those in the control arm at 12 weeks on the study (15% vs 9%, P = .00016)
Adverse events that were more common in the orteronel arm included nausea, fatigue, constipation, and diarrhea. More patients discontinued therapy in the orteronel arm compared with the control arm (30% vs 18%, respectively).
Forty-five percent and 51% of the orteronel-treated and control patients, respectively, went on to receive subsequent approved prostate cancer therapies including docetaxel, abiraterone, or enzalutamide.
The previously reported, phase III ELM-PC 5 trial of orteronel plus prednisone in previously treated mCRPC patients also showed an improvement in rPFS but not overall survival for men treated with orteronel.
According to Robert Dreicer, MD, MS, of the Taussig Cancer Institute at the Cleveland Clinic Lerner College of Medicine, and an author of the study, although there was previously clear evidence that orteronel was an active agent in prostate cancer, there was no prior evidence that orteronel could improve survival in chemotherapy-naive prostate cancer.
Orteronel is being developed by Takeda Pharmaceuticals and is a reversible inhibitor of 17,20-lyase, an enzyme involved in the production of androgens. The agent is a second-generation 17,20-lyase inhibitor, similar to abiraterone acetate, another 17,20-lyase inhibitor already approved for the treatment of men with metastatic prostate cancer.
“Many factors may have contributed to missing the objective [of this study], including subsequent therapy or the potential that orteronel is not as active a lyase inhibitor as abiraterone,” said Dreicer.
In the context of several active therapies for metastatic prostate cancer, overall survival is becoming a challenging endpoint to achieve, said Michael Morris, MD, associate professor at the Memorial Sloan-Kettering Cancer Center in New York, who was not involved in the study. “The environment in which we can actually see a survival advantage in any drug is becoming more difficult,” said Morris. “The outcomes really depend in many cases on the therapy patients in the trial cross over to receive after the clinical trial is completed. Whether or not this result is truly reflective of the drug activity is not clear.”
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.