(P004) Definitive Radiation in Early-Stage Endometrial Carcinoma
The purpose of this study is to describe the outcomes of definitive radiation in medically inoperable early-stage endometrial carcinoma. Although early-stage disease usually results in favorable overall survival (OS) after surgery, there is a growing cohort of patients who are medically inoperable secondary to morbid obesity.
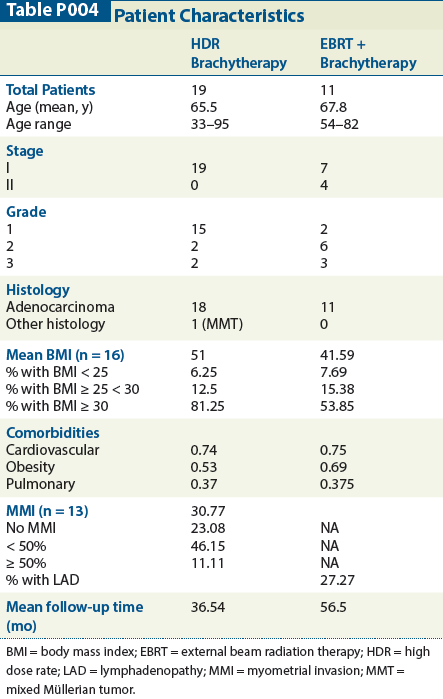
Table P004
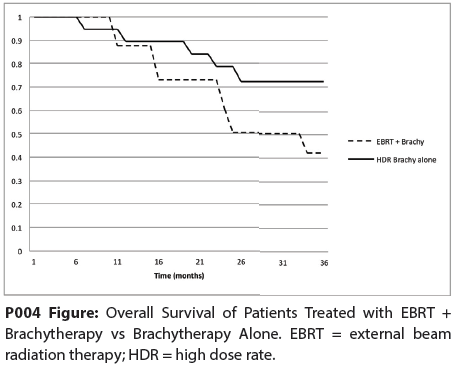
P004 Figure
Sahaja Acharya, MD, Kari Tanderup, PhD, Jacqueline Esthappan, PhD, Perry W. Grigsby, MD, MBA; Washington University
Introduction: The purpose of this study is to describe the outcomes of definitive radiation in medically inoperable early-stage endometrial carcinoma. Although early-stage disease usually results in favorable overall survival (OS) after surgery, there is a growing cohort of patients who are medically inoperable secondary to morbid obesity.
Methods: In this retrospective study, we analyzed the outcomes of 30 patients with International Federation of Gynecology and Obstetrics (FIGO) clinical stage I or II disease who were treated definitively between 2002 to 2011 with either high-dose–rate (HDR) brachytherapy to 36 or 48 Gy utilizing tandem, ovoids, and Simon-Heyman capsules or combined brachytherapy and external beam radiation therapy (EBRT). Prior to 2005, external beam radiation was delivered to the whole pelvis with a split field to a total dose of 50.4 Gy. After 2005, IMRT was utilized to deliver 50.4 Gy to the pelvic and para-aortic nodes and 20 Gy to the uterus or [18F]-fluoro-2-deoxy-D-glucose (FDG)-avid uterus if positron emission tomography (PET)/CT was available. The primary endpoint was overall survival (OS).
Results: Nineteen patients underwent HDR brachytherapy alone, all of whom were stage I. Eleven patients underwent brachytherapy and EBRT, 64% of whom was stage I. Mean follow-up time was 36.5 months in the brachytherapy group and 56.5 months in the combined modality group. Three-year OS was 72% in the brachytherapy group and 42% in the combined modality group (Figure). Patients who received combined modality therapy did have more advanced disease than those who received HDR brachytherapy alone. Two patients in the HDR brachytherapy group presented with symptomatic local recurrence at 7 months and at 2 years, respectively.
Conclusion: In conclusion, in our limited retrospective series, medically inoperable patients with FIGO clinical stage I endometrial carcinoma treated with modern-era HDR brachytherapy have a 3-year OS of 72% in the absence of surgery. Patients with more advanced disease have a worse outcome; however, it is unclear whether this is cancer-specific, as these patients have multiple comorbidities (listed in Table). Further investigation into cause-specific mortality in a larger cohort of patients is warranted.
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.