(P043) Stereotactic Radiosurgery Following Resection of Brain Metastases: Optimizing Benefit and Minimizing Risk
Postoperative radiation consolidation following resection of a symptomatic brain metastasis has traditionally been administered as whole-brain radiation therapy (WBRT). Given the increasing survival in some cancer patients, an increasing number of centers are offering postoperative cavity consolidation in the form of stereotactic radiosurgery (SRS).
P043 Figure
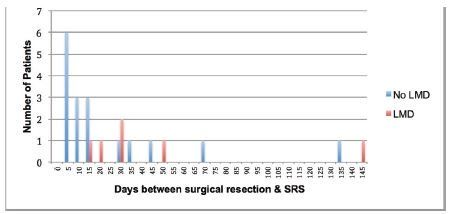
Table P043

Jennifer L. Quon, BS, Ryan A. Grant, MD, MS, CharlesE. Rutter, MD, James E. Bond, PhD, Veronica L. Chiang, MD; Yale University School of Medicine
Purpose: Postoperative radiation consolidation following resection of a symptomatic brain metastasis has traditionally been administered as whole-brain radiation therapy (WBRT). Given the increasing survival in some cancer patients, an increasing number of centers are offering postoperative cavity consolidation in the form of stereotactic radiosurgery (SRS). While there are anecdotal reports of success using this approach, whether SRS to the resection cavity alone can control intraoperative spill of tumor cells is not well established. We sought to determine our institutional rates of local control at the surgical site, as well as the rates of leptomeningeal dissemination, in patients treated with postoperative SRS consolidation.
Methods: We conducted a retrospective analysis of prospectively recorded data for all patients who underwent surgical resection of brain metastases, followed by consolidative SRS, at our institution between June 2007 and March 2013. All magnetic resonance (MR) imaging following SRS until death was reviewed for local recurrence and leptomeningeal disease (LMD). Patients without follow-up imaging were excluded. A univariate analysis was used to compare groups, and P < .05 was considered significant.
Results: A total of 23 patients were treated with SRS after surgical resection and had MR imaging follow-up. Primary pathology was melanoma in nine patients, lung cancer in four, breast in three, prostate in two, and colorectal carcinoma in one, and four had other cancer types. Median overall survival was 7.5 months (range: 2–51 mo) from surgical resection, with SRS administered at a median of 14 days post-resection (range: 3–143 d). Median resection cavity treatment volume was 13.8 cc (range: 3.1–42.9 cc). In addition to the surgical lesion, 17 patients (74%) had additional intraparenchymal lesions treated at the time of SRS, with a mean of 5 additional lesions per patient (range: 1–37). Treatment doses to the cavity margin ranged from 15–22 Gy (median 18 Gy). There were no cases of local tumor recurrence; however, four patients developed LMD between 131–1193 days after craniotomy. Their primary pathologies were breast cancer in two patients, squamous cell carcinoma in one, and melanoma in one. Two of the four patients had posterior fossa resections, and all four patients were treated with WBRT at time of LMD diagnosis. The patients with LMD received SRS on average 47 days after their surgical resection, compared with an average of 22.7 days for those without LMD
(P = .295).
Conclusions: LMD appears to occur as a result of systemic disease progression, as opposed to intracranial tumor spill at the time of resection, given the lengthy time interval between resection and LMD development in our sample. Given the 100% control rate of tumors in our resection cavities, we feel that SRS is a viable option for management of the postoperative resection bed. These findings will require further validation in a prospective trial.