Partial Nephrectomy Procedural Window Widened With Use of ICE Technique
A new technique of robotic partial nephrectomy has the potential for better preservation of kidney function and better cancer control during partial nephrectomy by allowing surgeons more time to perform the procedure compared with traditional open surgery, according to the results of a recently published case series.
A new technique of robotic partial nephrectomy has the potential for better preservation of kidney function and better cancer control during partial nephrectomy by allowing surgeons more time to perform the procedure compared with traditional open surgery, according to the results of a recently published case series.
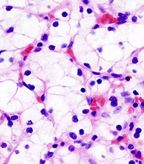
Histopathologic image of clear cell carcinoma of the kidney, nephrectomy specimen; source: KGH, Wikimedia Commons
Kidney cancer is a significant problem in the United States. The majority of people who undergo surgery for kidney cancer have the entire kidney removed, despite evidence of benefits of partial nephrectomy. In addition, the majority of kidney surgeries are done through a large, open incision, despite evidence of recovery benefits of a minimally invasive approach.
The new case series, published in European Urology, examined results from seven patients who underwent partial nephrectomy using intracorporeal cooling and extraction-or ICE-between April and September.
The key to the ICE approach was the use of a Gelpoint access port through which surgeons can introduce ice slush to the kidney using syringes. This technique means that after clamping, the kidney remains on ice as it would during open surgery.
“The study is the first to demonstrate a reliable and reproducible way of cooling the kidney by packing it in ice during robotic partial nephrectomy,” said Craig G. Rogers, MD, director of renal surgery at Henry Ford Hospital’s Vattikuti Urology Institute. “This helps minimize kidney damage while the blood supply to the kidney is temporarily clamped off to allow the tumor to be cut out and the kidney sewn back together.”
Surgeons can also remove the tumor to confirm gross margins while the kidney is still clamped, allowing them to remove more if needed while there is still time to do so, according to Dr. Rogers.
In the case series, robotic partial nephrectomy was achieved in all seven patients. The mean cold ischemia time was 19.6 minutes and the mean estimated blood loss was 296.4 mL. Final pathology results confirmed negative surgical margins for all cases.
“We know that minimally invasive partial nephrectomy is extremely challenging particularly within an approximate 30-minute time constraint of clamping off the blood supply, which limits broader application of the technique,” Rogers said. “These findings demonstrate feasibility of robotic partial nephrectomy using ice to cool the kidney, potentially extending the window of time surgeons have to work before kidney damage occurs.”
Rogers said that he and his colleagues hope that this technique will help more patients with kidney cancer realize the benefits of a partial nephrectomy and a minimally invasive approach.