Patient Adherence to Cancer Prevention Guidelines
In this interview we discuss how patient adherence to the American Cancer Society’s cancer prevention guidelines affects cancer risk and mortality.
Geoffrey Kabat, PhD, MS
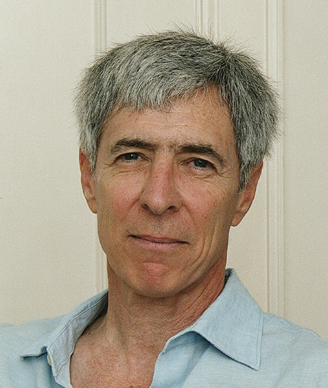
Today we are speaking with Geoffrey Kabat, PhD, MS, a cancer epidemiologist at the Albert Einstein College of Medicine in the Bronx, New York. Dr. Kabat and colleagues are the authors of a recent study in the American Journal of Clinical Nutrition that examined adherence to the American Cancer Society’s cancer prevention guidelines in relation to risk of cancer, cancer mortality, and total mortality.
-Interviewed by Anna Azvolinsky
Cancer Network: Dr. Kabat, can you talk a little about the American Cancer Society’s cancer prevention recommendations?
Dr. Kabat: In 2001, the American Cancer Society (ACS) issued a set of guidelines designed to reduce the risk of developing cancer. Other organizations have issued similar guidelines, but the ACS guidelines have been the most influential. The recommendations include maintaining a healthy body weight throughout life, being physically active, eating a healthy diet that emphasizes plant foods, and, if one drinks alcohol, limiting the amount of alcohol consumed. Another major recommendation is to avoid smoking.
Cancer Network: Could you tell us about the design and premise of the study you recently published?
Dr. Kabat: A number of studies have examined whether adhering to a set of guidelines, such as those of the ACS, is actually associated with improved health. However, for the most part, these studies focused on mortality, and only a small number examined the risk of major cancers-examined cancer incidence, in other words. We used data from the National Institutes of Health-AARP Diet and Health Study, which is a cohort of over half a million men and women between the ages of 50 and 71, to examine adherence to the ACS guidelines in relation to cancer risk, cancer mortality, and all-cause mortality. Participants were enrolled in 1995 to 1996 and were sent a detailed questionnaire covering diet, physical activity, weight, smoking history, and other factors. The cohort was followed from 10 to 13 years to identify cancers and deaths among participants. This is the largest study to have examined this question.
Now, in order to assess adherence to the guidelines, we created a score that assigned points for each of the components that we included in the questionnaire. Those are body weight, level of physical activity, alcohol consumption, and diet. So, for each component we assigned, say, 3 to 4 points, depending on the level of their responses, what their body weight or physical activity was, and so forth. And the dietary component included intake of whole grains, fruits and vegetables, and meat. So then once we assigned points to each component, we summed the points’ total for each participant and that was examined in relationship to the outcomes. The large size of the study allowed us to look at specific cancer sites and to look at performance of the score in never-smokers, former smokers, and current smokers. This is important because smoking is such a strong risk factor for many cancers and for total mortality, and one wants to do the best one can to remove its effect, to assess the contribution of these other factors.
Cancer Network: What were the main findings? And was anything particularly surprising?
Dr. Kabat: We found that, compared with those with the lowest level of adherence, those with the highest level of adherence had a modest reduction in cancer incidence, 10% in men and 19% in women. In addition, men with the highest adherence had a 25% reduction in their risk of dying from cancer, and the corresponding figure for women was 24%, so very similar for men and women. Finally, men with the highest level of adherence had a 26% reduction in their overall risk of dying, compared with a 33% reduction in women. In addition to looking at the risk of developing cancer generally, owing to the large number of participants, we were able to look at the association with the risk of cancer at 25 specific anatomic sites. This is a novel aspect of the study. There we found something that did surprise us. We found 14 sites where people adhering most closely to the guidelines had reduced risks for developing cancer compared with those in the lowest adherence group. Notable examples were gallbladder cancer-65% reduction, endometrial cancer-60% reduction, liver cancer-48% reduction in males, colon cancer-48% reduction in males and 35% in females, and rectal cancer-40% reduction in males and 36% in females. But adhering to the guidelines was not always associated with lower risk. Compared with the least adherent men, the most adherent men had a statistically significant 19% greater risk of developing melanoma, although the reason for this was unclear. For other sites, there was no association with adherence. Thus, we see striking differences between cancer sites.
Cancer Network: This was an observational study, so what can we take away from these results and what are the study’s limitations?
Dr. Kabat: This is an important point. It’s important to recognize the limitations of observational studies, like the present one. This is the best we can do to address this type of question, because it would not be feasible to conduct a clinical trial in which you randomized subjects to different groups with different levels of adherence. However, we know from extensive experience that people with certain health behaviors may differ in important ways from people who do not practice these behaviors. Famously, in observational studies women who used hormone therapy were different in many ways from women who didn’t, and this led to erroneous conclusions about the benefits of hormone therapy. Therefore, we have to be careful not to interpret these results as proof that if one were to follow the ACS guidelines, one would reduce one’s risk of cancer and of death.
People who practice more healthy behaviors are apt to be generally more health-conscious than those who are less adherent, and this might entail other habits and behaviors that are responsible for their better outcomes. We know that many different behaviors tend to be correlated. So, some factor other than the ones we examined might be responsible for the observed reductions in risk. Now, we only found a modest overall reduction in cancer incidence, but a larger reduction in cancer mortality and, particularly, overall total mortality. And the latter suggests that people who are more adherent may have access to higher-quality medical care, and this may, in part, account for their improved mortality. Or maybe people who are more adherent are more educated and better off economically and, for these reasons, may do better in terms of these outcomes. Differences of this sort may persist even though we tried to adjust for various factors, such as educational level. This is an important caveat to keep in mind. However, having said that, I should also say that there is extensive evidence from different observational studies in different populations, as well as from clinical trials, which consistently suggests that maintaining a healthy body weight, being physically active, not over-consuming alcohol, and eating a plant-centered diet is associated with better health.
Cancer Network: How do these results compare with other similar studies?
Dr. Kabat: The results of our study are quite consistent with those from a handful of other studies that have assessed the impact of health guidelines issued by different organizations. As in our study, these studies suggest a stronger impact on overall mortality than on cause-specific mortality.
Cancer Network: Are you currently working on a follow-up to this study?
Dr. Kabat: A colleague in our department, Dr. Chelsea Catsburg, is doing a number of similar analyses focused on breast and colorectal cancer mortality. In addition, we are pursuing many related questions having to do with lifestyle behaviors and characteristics, including body weight and body fat distribution in relation to effects on metabolism and inflammation, and cancer.
Cancer Network: What can oncologists learn from this and other such studies, and perhaps apply to their own practice?
Dr. Kabat: As I said, I think our results are in line with a wealth of studies of different types. But what comes to mind specifically is a recent study published in Science, which has created quite a stir and purports to show that two-thirds of cancers may be due to random mutations-that is, that only a minority of cancers are attributable to lifestyle/environmental exposures or to heredity. That estimate is likely to be greatly inflated. The wide range of variation in cancer rates internationally and the substantial reductions we observed for many common cancers suggest that modifiable factors, while certainly not the whole story, play an important role in cancer.
Cancer Network: Thank you so much for joining us today, Dr. Kabat.
Dr. Kabat: You’re very welcome.
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.