Pazopanib Induces ‘Clinically Meaningful Activity’ in Refractory Urothelial Cancer
The antiangiogenic agent pazopanib demonstrated clinically meaningful activity in patients with refractory urothelial cancer in a phase II proof-of-concept study, identifying pazopanib as the first targeted compound to have clinically meaningful activity in patients with refractory urothelial cancer.
CHICAGO-The antiangiogenic agent pazopanib demonstrated clinically meaningful activity in patients with refractory urothelial cancer in a phase II proof-of-concept study, reported Andrea Necchi, MD, faculty member in the department of medicine at Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy. Dr. Necchi said data from the trial identify pazopanib as the first targeted compound to have clinically meaningful activity in patients with refractory urothelial cancer (AACR abstract LB-433).
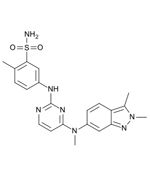
Chemical structure of pazopanib
Pazopanib (Votrient) is a potent and selective multi-targeted receptor tyrosine kinase inhibitor. It is currently approved by the US Food and Drug Administration for use in renal cell carcinoma.
“Our data indicate that pazopanib seems to be a legitimate drug in this disease,” said Dr. Necchi. “Historically, prognosis of patients with relapsed or refractory urothelial cancer is quite dismal. Patients who fail to be cured after multiple chemotherapy regimens have a poor survival estimate, and palliative care is a reasonable trade-off.”
The researchers assigned 41 patients with relapsing or progressing urothelial cancer between 2010 and 2011 to 800 mg once-daily pazopanib. All patients had at least one prior chemotherapy regimen for metastatic disease.
At follow-up, 7 patients had a partial response to therapy and 24 patients had stable disease-an overall clinical benefit of 76%. Median progression-free survival was 2.6 months, and median overall survival was 4.7 months; 10% of patients, however, had a long-term cure after a median follow-up of 19 months.
Promising interim results of the study were reported previously (ESMO 2010, ASCO 2011). Dr. Necchi presented final results corroborated by biomarker analysis. The investigators examined blood samples for predictive biomarkers at baseline and every 4 weeks. “Most interestingly, our biomarker analysis clearly pointed out the role of rising levels of circulating interleukin-8 (as measured after 4 weeks of therapy) as an early and potentially practice-changing indicator of tumor resistance and poor survival,” he noted. Rising levels were in fact associated with disease progression as assessed by CT scan and shorter survival.”
“This trial gave a clear proof of concept that will require confirmation on a larger number of patients,” said Dr. Necchi. “However, the preliminary findings, mainly regarding the role of interleukin-8 levels, have the potential to change at least the concept of new trial design with antiangiogenic agents in this disease.
“This is the first trial ever presented to meet the primary end point with a targeted drug in urothelial cancer,” he concluded. “A role for antiangiogenesis in urothelial cancer has been set in a population of highly pretreated patients. The clinical data merit to be challenged in a larger, confirmatory trial while the results on IL-8 might help in shaping more personalized trials with antiangiogenic compounds in the near future. IL-8 might be also a further target for treatment.”
The study was sponsored by Fondazione IRCCS Istituto Nazionale dei Tumori. GlaxoSmithKline Inc. provided the drug supply and granted independent radiologic review, which was performed at Columbia University Medical Center.