PCV Added to Radiation Therapy Improves Survival Most in Low-Grade Glioma Subtypes
The addition of procarbazine, CCNU, and vincristine to RT in patients with low-grade glioma prolongs progression-free and overall survival vs RT alone.
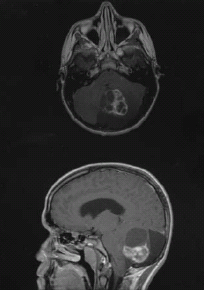
Resectable low-grade glioma
The addition of procarbazine, CCNU, and vincristine (PCV) to radiation therapy (RT) in patients with low-grade glioma prolongs both overall and progression-free survival compared with RT alone, in particular among the oligodendroglioma and oligoastrocytoma histologic subtypes, according to a new study presented at the Society for Neuro-Oncology (SNO) Annual Scientific Meeting in Miami.
Grade II gliomas are a relatively uncommon malignancy, representing between 5% and 10% of brain tumors, said Jan C. Buckner, MD, of the Mayo Clinic, in Rochester, Minnesota. Though these are slow-growing tumors, Buckner said that “nearly all patients eventually develop neurological decline and premature death.”
Recent results from the R9802 trial showed that PCV along with RT at the time of initial diagnosis provides significant overall and progression-free survival benefit in all patients in the trial. The trial began in 1998, and finished accrual in 2002 (251 patients); follow-up has continued since then, with most recent results showing dramatic improvements with PCV at the American Society of Clinical Oncology (ASCO) Annual Meeting in June. At that time, the median progression-free survival with RT alone was 4 years vs 10.4 years with the addition of PCV. Similar improvement in overall survival was seen, at 7.8 years vs 13.3 years. All patients in the trial were either over 40 years of age at diagnosis or with less than total resection.
The current analysis divided the outcomes by histologic subtype. The hazard ratio (HR) for survival showed significant overall survival improvement in oligodendroglioma (HR = 0.43) and oligoastrocytoma (HR = 0.56); there was indication of benefit in astrocytoma as well, but it did not reach significance (HR = 0.73; P = 0.31).
The survival rates were better with PCV at 5 years, but that difference was larger at 10 years. There was a 22% improvement in survival at 10 years in oligodendroglioma patients, a 26% improvement in oligoastrocytoma, and a 16% improvement in astrocytoma. In the full cohort, PCV yielded an increase in survival of 20% at 10 years.
Though there was increased toxicity in the PCV group compared with RT alone, Buckner said it was relatively well tolerated. Only three patients required red blood cell transfusions, and only one required a platelet transfusion. There were no treatment-related deaths. Late radiation toxicities were also infrequent.
“The improved survival is apparent in all histologic subtypes, but the treatment effect is greatest for those with oligodendroglioma and oligoastrocytoma, for whom it is statistically significant,” Buckner concluded. In the future, he added, his group will assess outcomes by molecular markers, focusing in particularly on IDH mutations and 1p/19q co-deletion. “We postulate that … those without either of those alterations are likely to be chemo-resistant.”