Personalized Genetic Testing Fails to Improve CRC Screening Rates
People who underwent genetic and environmental risk assessment evaluating their colorectal cancer risk were no more likely to undergo screening for the disease.
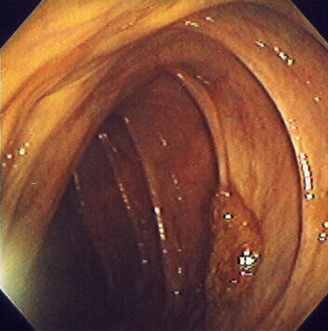
Sessile colon polyp; source: Stephen Holland, MD, Wikimedia Commons.
People at average-risk for colorectal cancer (CRC) who underwent genetic and environmental risk assessment (GERA) to evaluate their risk for CRC were no more likely to undergo CRC screening than those people who did not receive this individualized assessment, results of a study showed.
Additionally, among those people who underwent GERA, those told that they were at elevated risk for CRC were no more likely to undergo screening than those told to be at average risk.
“Further study is required to assess whether other such information and different means of presenting individualized results for common diseases like CRC will spur more healthy behaviors to reduce risk,” researchers led by David S. Weinberg, MD, MSc, of Fox Chase Cancer Center, and colleagues wrote in Annals of Internal Medicine.
In an editorial that accompanied these results, J.S. Blumenthal-Barby, PhD, MA, and Amy L. McGuire, JD, PhD, both of Baylor College of Medicine, and Peter A. Ubel, MD, of Duke University, wrote that these results were surprising and indicate that physicians will need to look beyond genomic medicine to persuade people to participate in practices such as CRC screening.
“We should not look toward personalized medicine and genomics to refine risk estimates in ways that will, on their own, motivate substantial behavior change,” they wrote. “Instead we should utilize such information to identify patients who are most in need of such screening and then rely on proven persuasion techniques to encourage patients to get screened.”
In the study, Weinberg and colleagues randomly assigned 783 patients who were not adherent to screening at study entry to usual care or GERA, which evaluated methylenetetrahydrofolate reductase polymorphisms and serum folate levels. Patients who received GERA were told that they were at either elevated or average risk for CRC.
About one-third of patients in both groups underwent CRC screening within 6 months of study entry (35.7% for usual care vs 33.1% for GERA). Within the GERA group, 38.1% of average-risk patients and 26.9% of elevated-risk patients underwent screening.
The researchers did note an increase in “knowledge about CRC screening and the role of genetic risk, suggesting that the educational component of the intervention was successful.” But they also noted that there was no association between baseline or post-intervention knowledge and the likelihood of a patient undergoing screening.