PET-CT Outperforms CT in Follicular Lymphoma
Data from a pooled analysis show that PET-CT provided better response assessment than did CT and predicted inferior survival in follicular lymphoma patients.
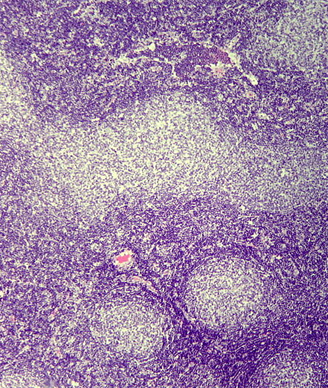
Follicular lymphoma, H&E stain; source: Patho, Wikimedia Commons
Data from a pooled analysis has shown that combined FDG PET-CT provided better response assessment than did conventional contrast-enhanced CT in follicular lymphoma patients, and PET-CT was able to predict inferior progression-free and overall survival after first-line rituximab.
Results published in Lancet Haematology, showed that patients with a positive PET-CT scan after rituximab treatment had significantly greater risk for progression and death compared with patients with a negative scan.
“Although these results are reassuring for patients who have a negative PET scan, those who have a positive PET scan after first-line therapy can no longer be regarded as having an indolent disease and should be closely monitored,” wrote Judith Trotman, MD, of the University of Sydney, Australia, and colleagues. “We expect post-induction PET assessment will be a platform for studies of response-adapted therapy aimed to improve the poor prognosis of patients with a positive post-induction PET scan.”
Trotman and colleagues conducted a pooled analysis of three multicenter studies of first-line rituximab in patients with high-tumor burden follicular lymphoma: the PRIMA study, the PET-Folliculaire study, and the Fondazione Italiana Linfomi FOLL05 study. Patients enrolled in these studies underwent at least 6 cycles of rituximab and chemotherapy before response assessment with either conventional CT or PET-CT. The research included patients who received a PET scan within 3 months of their last rituximab dose.
For the study, three reviewers reviewed PET images and scored them using the Deauville scale; a PET scan was considered positive with a score of 4 or more points on the scale.
Of the 439 patients included in this assessment, 246 had centrally reviewed post-induction scans. Positive PET was found in 17% of patients.
At a median follow-up of 54.8 months, the hazard ratio for progression-free survival for a positive PET scan compared with a negative PET scan was 3.9 (95% CI, 2.5-5.9; P < .0001); the hazard ratio for overall survival was 6.7 (95% CI, 2.4-18.5; P = .0002).
At 4 years, the progression-free survival in patients with a positive scan was 23.2% compared with 63.4% for those with a negative scan (P < .0001). The 4-year overall survival was 87.2% for positive scans compared with 97.1% for negative scans (P < .0001).
“A negative post-induction scan in 83% of patients predicts a median progression-free survival beyond 6 years,” the researchers wrote. “Conversely, patients who had a positive post-induction PET scan had a median progression-free survival of only 17 months, with an increased risk of death, identifying a population for whom follicular lymphoma can no longer be characterized as indolent.”
In an accompanying editorial, Bruce D. Cheson, MD, of Georgetown University Hospital Lombardi Comprehensive Cancer Center, pointed out that although this new information is valuable, it is not yet clear what physicians will do with it.
“In clinical practice, patients with a positive scan could be followed up more closely,” Dr. Cheson wrote. “No data yet show that intervention with treatment after a positive PET result in patients with follicular lymphoma will improve outcome.”
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.