Phase 3 IDeate-Esophageal01 Trial Initiated for Unresectable ESCC
The trial initiation is based on phase 1/2 IDeate-PanTumor01 trial results presented at the 2022 and 2023 European Society for Medical Oncology Congress.
Results from the phase 1/2 trial revealed that among 118 patients treated with 4.8 mg/kg to 16.0 mg/kg of I-DXd for solid tumor indications—including ESCC, among others—an objective response rate of 32% was observed, with a confirmed response rate of 28%.
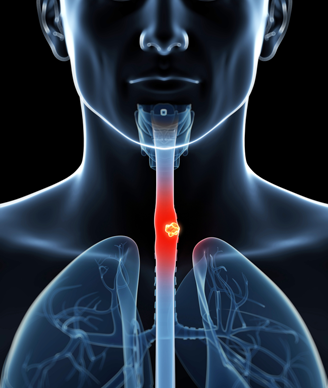
Investigators have dosed the first patient in the phase 3 IDeate-Esophageal01 trial (NCT06644781) assessing the efficacy of ifinatamab deruxtecan (I-DXd) in patients with unresectable advanced or metastatic esophageal squamous cell carcinoma (ESCC), according to a news release from the drug’s developer, Merck.1
Of note, the initiation of the phase 3 IDeate-Esophageal01 trial is based on results from the phase 1/2 IDeate-PanTumor01 study (NCT04145622), in which the investigational therapy was assessed in patients with advanced solid malignant tumors. The results for the trial were presented at the 2022 and 2023 European Society for Medical Oncology (ESMO) Congress.
Results from the phase 1/2 trial revealed that among 118 patients treated with 4.8 mg/kg to 16.0 mg/kg of I-DXd for solid tumor indications—including non–small cell lung cancer (NSCLC), small cell lung cancer (SCLC), castration-resistant prostate cancer (CRPC), and ESCC, among others—an objective response rate (ORR) of 32% (95% CI, 24%-41%) was observed.2 In total, 28% (95% CI, 20%-37%) of responses were confirmed.
“Advanced ESCC is a difficult-to-treat disease, and unfortunately overall survival [OS] remains low,” Marjorie Green, MD, senior vice president and head of Oncology, Global Clinical Development at Merck Research Laboratories, said in the news release.1 “The initiation of the pivotal phase 3 IDeate-Esophageal01 clinical trial demonstrates our shared commitment with Daiichi Sankyo to further expand our clinical development program evaluating this potentially first-in-class antibody drug conjugate [ADC] across multiple solid tumors where there are unmet needs for new treatment options.”
Patients in the phase 3 trial will be randomly assigned to receive either I-DXd or an active comparator, which includes either docetaxel, paclitaxel, or irinotecan hydrochloride. Those in the experimental arm will receive 12 mg/kg of intravenous I-DXd on day 1 of 21-day cycles.3 Those in the comparator arm will receive an intravenous infusion of investigator’s choice of chemotherapy. The target enrollment for the phase 3 trial is 510 patients.
The primary end point of the phase 3 trial is OS. Secondary end points include progression-free survival, ORR, duration of response, disease control rate, and safety.
Ifinatamab deruxtecan is specifically engineered as a potential B7-H3–directed DXd ADC. It was initially discovered by Daiichi Sankyo and is being jointly developed by Merck.
“Patients with metastatic ESCC continue to experience poor outcomes despite currently available treatments,” Mark Rutstein, MD, head of Therapeutic Area Oncology Development at Daiichi Sankyo, stated in the news release.1 “The encouraging clinical activity seen in our early-phase signal finding trial supports further evaluation of ifinatamab deruxtecan as a potential treatment strategy for these patients.”
Patients eligible for study enrollment are 18 years and older; have histologically confirmed or cytologically documented unresectable locally advanced or metastatic ESCC; have disease progression following a platinum-based chemotherapy regimen and an immune checkpoint inhibitor therapy; and have provided adequate baseline tumor samples. Additionally, patients must have at least 1 measurable lesion on CT or MRI according to RECIST v1.1 criteria and an ECOG performance status or 0 or 1 within 7 days of treatment start.
Patients are excluded from trial enrollment if they: have received prior orlotamab (MGD009), enoblituzumab (MGA271), or other B7-H3–targeted agents; have received any prior topoisomerase inhibitor; have histologically confirmed or cytologically documented adenosquamous carcinoma subtype; or are ineligible for all chemotherapies in the comparator arm. Those with tumor invasion into organs adjacent to the esophageal disease site, clinically active central nervous system metastases, or clinically significant corneal disease are also excluded.
References
- IDeate-Esophageal01 phase 3 trial of ifinatamab deruxtecan initiated in certain patients with pretreated advanced or metastatic esophageal squamous cell carcinoma. News release. Merck. May 19, 2025. Accessed May 19, 2025. https://tinyurl.com/4txvf3t4
- DS-7300 continues to show promising durable response in patients with several types of advanced cancer. News release. Daiichi Sankyo. September 10, 2022. Accessed May 19, 2025. https://tinyurl.com/5x93h3zy
- A study of ifinatamab deruxtecan in subjects with pretreated advanced or metastatic esophageal squamous cell carcinoma (ESCC) (IDeate-Esophageal01). ClinicalTrials.gov. Updated May 14, 2025. Accessed May 19, 2025. https://tinyurl.com/25dczdtw