Post-Remission Allogeneic HSCT Preferred in Older AML Patients
Allogeneic HSCT may be the best treatment option in older patients with acute myeloid leukemia who obtain first complete remission after induction chemotherapy.
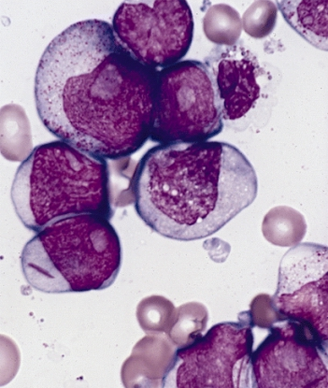
Bone marrow smear from a patient with acute myeloid leukemia
Allogeneic hemopoietic stem cell transplantation (HSCT) may be the best treatment option in older patients with acute myeloid leukemia (AML) who obtain first complete remission after induction chemotherapy.
A study published recently in Lancet Haematology compared allogeneic HSCT with no post-remission treatment and multiple other post-remission treatment strategies and showed it to improve survival, especially in patients with adverse-risk AML.
“Although transplant decisions should be based on a careful pre-transplant risk assessment of relapse and non-relapse mortality, these results suggest that the early search and identification of a compatible donor should also be pursued in elderly patients with an adverse AML risk profile,” wrote Jurjen Versluis, MD, of the Erasmus University Medical Center Cancer Institute in the Netherlands, and colleagues.
According to the study, although many older patients with AML will enter first complete remission, often no post-remission therapy is offered. In this time-dependent analysis, Versluis and colleagues sought to determine how allogeneic HSCT compared with forgoing post-remission treatment or undergoing treatment with other options.
The researchers used results taken from four HOVON-SAKK AML trials, which included 1,155 patients aged 60 or older. The 640 patients from these trials who had first complete remission after induction chemotherapy were included in this analysis.
Patients underwent a variety of post-remission therapies: allogeneic HSCT following reduced-intensity conditioning (n = 97), gemtuzumab ozogamicin (n = 110), chemotherapy (n = 44), autologous HSCT (n = 23), or no further treatment (n = 366). The primary endpoint of the analysis was 5-year overall survival.
Patients who underwent allogeneic HSCT had a 5-year overall survival of 35% compared with 21% in those who had no additional post-remission treatment (P = .033) and 26% in those who had additional chemotherapy or autologous HSCT. A similar benefit was seen for relapse-free survival. Those patients who underwent allogeneic HSCT had a 5-year relapse-free survival of 32% compared with 14% in those patients who had no post-remission treatment (P = .007) and 20% for other post-remission therapies.
The researchers found that patients who had favorable risk, as defined by the European Leukemia NET AML risk score, had a better 5-year overall survival compared with those with intermediate or adverse risk (56% vs 23% vs 13%).
When Versluis and colleagues conducted a multivariable analysis with allogeneic HSCT as a time-dependent factor they found that allogeneic HSCT was associated with an improved 5-year overall survival compared with other post-remission therapies and no post-remission therapy (hazard ratio [HR], 0.71 [95% confidence interval (CI), 0.53–0.95]; P = .017). This improvement in overall survival was greatest in patients classified as intermediate risk (HR, 0.82 [95% CI, 0.58–1.15]) and advanced-risk (HR, 0.39 [95% CI, 0.21–0.73]). No difference in the favorable-risk group was seen because of the small number of these patients in the study group, the researchers wrote.
There was a 5-year cumulative incidence of non-relapse mortality of 18% after allogeneic HSCT compared with 14% in patients receiving no allogeneic HSCT and 9% in those receiving other post-remission treatments. This outcome “could compromise the favorable effects of allogeneic HSCT on relapse, especially in elderly patients with comorbidities,” the researchers acknowledged.
In an editorial that accompanied the study, Marcos de Lima, MD, of Case Western Reserve University, Cleveland, Ohio, discussed a couple of points related to the study. First, he mentioned that the proportion of patients in this study undergoing transplant was low, likely a reflection of the years the study was conducted. More recent reports suggest that the use of allogeneic transplant increased after the year 2006, he wrote.
“Another recent development that adds complexity and hope is the availability of donors for most patients. This statement presumes that haploidentical and cord blood donors assure an allogeneic graft to all,” de Lima wrote. “Preliminary retrospective studies indicate similar outcomes using such alternative donors. If equivalence or comparability of results is assumed, it challenges the classic donor vs no donor approach used in genetic randomization studies, which relies on well-matched related or unrelated donor availability.”
Overall, de Lima agreed with Versluis and colleagues that the results need to be confirmed in a randomized trial. Until then, he recommended “allogeneic transplantation as a suitable post-remission therapy to fit patients aged 60 years and older with intermediate-risk or high-risk AML in first remission who have a matched related or unrelated donor.”