Post-Treatment Lymphedema Common in Breast Cancer Patients
Sharon Krumm, PhD, RN, the Editor of Oncology Nursing, is administrator and director of nursing, Johns Hopkins Oncology Center, and assistant professor, Johns Hopkins University Schools of Medicine and Nursing. ONI is pleased to announce the creation of an Editorial Advisory Board for Oncology Nursing. Members are Catherine Coleman, RN, OCN, a consultant for breast center development, Tiburon, California, and Mary McCabe, BSN, MA, acting director, Office of Communications, National Cancer Institute, Be-thesda, Maryland. See p. 27 for more about the board members.
Sharon Krumm, PhD, RN, the Editor of Oncology Nursing, is administrator and director of nursing, Johns Hopkins Oncology Center, and assistant professor, Johns Hopkins University Schools of Medicine and Nursing. ONI is pleased to announce the creation of an Editorial Advisory Board for Oncology Nursing. Members are Catherine Coleman, RN, OCN, a consultant for breast center development, Tiburon, California, and Mary McCabe, BSN, MA, acting director, Office of Communications, National Cancer Institute, Be-thesda, Maryland. See p. 27 for more about the board members.
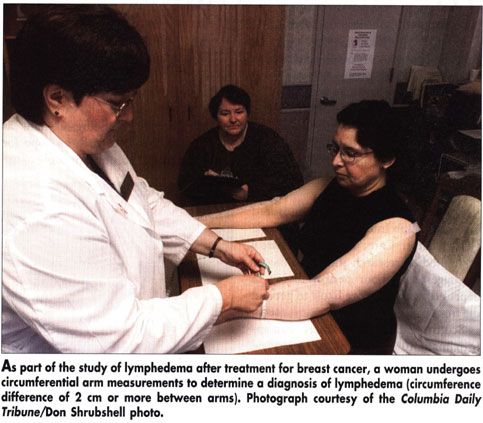
WASHINGTONLymphedema in breast cancer survivors is more common and more disabling than generally believed, according to Jane M. Armer, RN, PhD. In a poster presented at the Oncology Nursing Society’s 27th Congress (abstract 187), Dr. Armer reported that in a group of women who were an average of 3 years post-treatment for breast cancer, 39% had a circumference difference of 2 cm or more between arms (sufficient for a diagnosis of lymphedema), and 40% had a difference of between 1 and 2 cm, which some consider latent lymphedema.
The descriptive-correlational, cross-sectional study included 103 women treated for breast cancer at a midwestern medical center. Mean age was 59 years (range, 31 to 88 years). Mean time since diagnosis was 3 years (range, 3 months to 41 years). A high proportion of these women reported signs and symptoms of lymphedema. Forty of the 103 women developed lymphedema as defined above. Two thirds (63%) of these women reported swelling, 60% had limb heaviness, 45% had tenderness, and 38% had numbness (see Table 1). Of all 103 women receiving treatment, 55% reported current numbness, and 42% reported limb tenderness in the past year (see Table 2).
Dr. Armer, associate professor, University of Missouri-Columbia Sinclair School of Nursing and director of nursing research, Ellis Fischel Cancer Center, found that women with lymphedema had significantly more swelling and heaviness, while reports of numbness and tenderness in the lymphedema group and the total group did not differ significantly.
"Post-breast cancer lymphedema is a chronic, distressful symptom that is poorly understood, acknowledged, and addressed by health providers," Dr. Armer said. This was illustrated by the study subject who, 41-years after her diagnosis, said, "Going through treatment for breast cancer was nothing compared to 39 years with lymphedema."
The researchers found that most of the study subjects did no self-care activities to manage their signs and symptoms. Dr. Armer said that the investigators have completed work comparing circumferences, water displacement, and infrared laser perometry assessments of limb volume in healthy women and in breast cancer survivors, with the goal of developing an assessment tool to score risk and guide recommendations for self-care.