Potential Targets of Lung Squamous Cell Carcinoma Revealed in Genetic Analysis
A recent study profiling the genetic details of 178 lung squamous cell carcinomas yielded a clearer picture of the mutations that characterize the disease, and potentially revealed therapeutic targets.
A recent study profiling the genetic details of 178 lung squamous cell carcinomas yielded a clearer picture of the mutations that characterize the disease, and potentially revealed therapeutic targets. Squamous cell carcinomas kill about 400,000 people around the world every year.
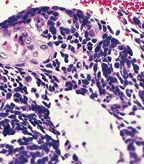
Combined small cell lung carcinoma (with squamous cell carcinoma); source: Wikimedia Commons
A large group of researchers acting as part of the Cancer Genome Atlas Research Network, including Matthew Meyerson, MD, PhD, of the Dana Farber Cancer Institute in Boston, analyzed samples from 178 patients with previously untreated stave I-IV lung squamous cell carcinoma (SQCC); the results were published in Nature. Consistent with previously reported rates, 96% of the cohort had a history of tobacco use.
The overall analysis revealed a wide array of DNA alterations in the SQCC tumors. The SQCCs had a mean of 360 exonic mutations, 323 altered copy number segments and 165 genomic rearrangements per tumor. Ten significantly mutated genes were identified, and TP53 mutation was found in as many as 90% of the samples, similar to high-grade serous ovarian carcinomas.
“Many of the somatic alterations we have identified in lung SQCCs seem to be drivers of pathways important to the initiation or progression of the cancer,” the authors wrote. “Specifically, genes involved in the oxidative stress response and squamous differentiation were frequently altered.”
The researchers looked specifically for therapeutic targets as well. “Molecularly targeted agents are now commonly used in patients with adenocarcinoma of the lung, whereas no effective targeted agents have been developed specifically for lung SQCC,” they wrote. They found that 96% of the tumors contained one or more mutations in tyrosine kinases, serine/threonine kinases, proteases, or other commonly targeted proteins.
More specific analysis showed that 69% of samples had alterations to either the PI(3)K/AKT, receptor tyrosine kinase (RTK), or RAS pathways. One component of the PI(3)K/AKT pathway was mutated in 47% of patients; 26% of tumors had RTK signaling affected by EGFR or FGFR amplification or BRAF mutation. Notably though, the most common mutations in lung adenocarcinomas-EGFR and KRAS mutations-were found in almost none of the SQCC samples.
The study also found a previously unreported loss-of-function mutation in the HLA-A class I major histocompatibility gene, which the authors wrote matches the “cancer hallmark of avoiding immune destruction.” The presence of the loss-of-function mutation suggests there could be a role for genotypic selection of patients who are candidates for immunotherapies.
“The current study has identified a potentially targetable gene or pathway alteration in most lung SQCC samples studied,” the authors wrote. The new genetic information found in this study “can help to organize efforts to analyze lung SQCC clinical tumor specimens for a panel of specific, actionable mutations to select patients for appropriately targeted clinical trials. These data could thereby help to facilitate effective personalized therapy for this deadly disease.”