Prostate Cancer Risk Higher in Obese Men After Benign Biopsy
A case-control study of almost 500 men suggests that obese men who have had a benign prostate biopsy have a greater risk of prostate cancer in the future.
A case-control study of almost 500 men suggests that obese men who have had a benign prostate biopsy have a greater risk of prostate cancer in the future.
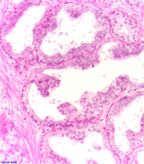
Microscopic view of prostatic intraepithelial neoplasia; note atypical epithelial cells; no malignant, infiltrating neoplasia visible; source: Alex Brollo, Wikimedia Commons
After accounting for family history of prostate cancer, prostate-specific antigen (PSA) levels, and other variables, the study found that men who were obese at the time of biopsy had a 57% increased incidence of prostate cancer during follow-up, while those who were overweight had a 44% increased incidence of prostate cancer.
Obesity was not associated with high-grade tumors in this study, but rather with low-grade tumors. This result, however, was not statistically significant and may be a reflection of chance or the type of cohort studied.
Andrew Rundle, associate professor of epidemiology at Columbia University Mailman School of Public Health, New York, and colleagues found that men who were obese were more likely to have precancerous lesions detected in their benign prostate biopsies compared with men who were not obese. The obese men were at a greater risk for developing prostate cancer after their biopsy. The study, according to the researchers, is the first attempt to analyze the potential link between precancerous abnormalities in the prostate and obesity. The results are published in Cancer Epidemiology, Biomarkers & Prevention.
Identifying risk factors for prostate cancer remains an important goal for researchers and clinicians. Approximately 1 million men undergo biopsies to test for prostate cancer each year in the United States, and about 25% are diagnosed with the disease.
From a cohort of 6,692 men who had an initial benign biopsy, the study focused on 494 men within the cohort and 494 controls who had not had a biopsy. From this group, prostatic intraepithelial neoplasia (PIN) was detected in 11% of the benign biopsy study participants. Obesity was significantly associated with PIN at the time of the biopsy.
Those men who were obese were more likely to be diagnosed with cancer and had a 57% increased rate of prostate cancer within approximately 4.2 years of the benign biopsy.
Obesity was defined as a body mass index (BMI) of 30 or higher, while a BMI between 25 and 30 was considered to be overweight status.
The authors noted that the association between obesity and prostate cancer risk was higher compared with two previous studies-this could be either due to chance or the cohort studied.
The sensitivity of needle biopsies is generally lower for obese men because they have larger prostates, making it more difficult to detect small tumors. A tumor may be missed during the initial biopsy and detected in a biopsy early in the follow-up period. This would be consistent with the results of this study that show obese men are more likely to be diagnosed with cancer within a shorter time frame from the initial benign biopsy.
Currently, physicians do not alter biopsy procedures due to a patient’s BMI. There are risk models, however, that incorporate BMI as a factor to calculate an individualized prostate cancer risk, as studies show obesity can lower the sensitivity of PSA testing. Rundle has developed a PSA calculator that adjusts a man’s PSA score based on their BMI.
“We need some guidance on when or for whom a full follow-up is required,” said Rundle in a press release. “Obesity should be considered a factor for more intensive follow-up after a benign prostate biopsy.”
Rundle and colleagues are now studying whether prostate size is related to inflammation and obesity, and whether this can explain the link of these factors to prostate cancer risk.