PSA Testing Declining Faster With Primary Care Physicians Than Urologists
The 2012 change in guidelines regarding PSA testing for prostate cancer had a different effect on testing rates depending on which physician specialty was doing the testing.
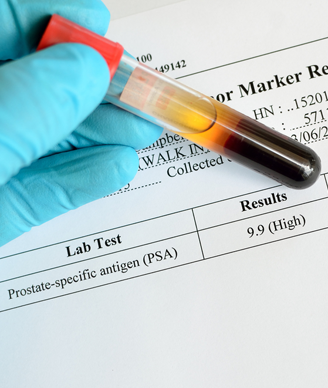
Image © Jarun Ontakrai / Shutterstock.com
The 2012 change in guidelines regarding prostate-specific antigen (PSA) testing for prostate cancer had a different effect on testing rates depending on which physician specialty was doing the testing, according to a new study. Primary care physicians showed a marked decline in PSA tests administered, while urologists had only a slight drop in testing.
The use of PSA testing was and remains controversial. In May 2012 the US Preventive Services Task Force (USPSTF) recommended against the test to detect prostate cancer in men, writing that “there is moderate certainty that the benefits of PSA-based screening for prostate cancer do not outweigh the harms.”
The new study, led by Michael E. Zavaski, MD, of Brigham and Women’s Hospital in Boston, compared PSA testing rates based on the National Ambulatory Medical Care Survey in 2010 and 2012. They included a total of 1,222 physician visits, including 113 to urologists and 1,109 to primary care physicians (PCPs). These visits (after exclusions for men with a diagnosis of prostate cancer or other prostate disorders) were weighted to reflect the US population, yielding a weighted sample of 27 million total visits of which 800,000 were to a urologist. The results of the survey were published online ahead of print in JAMAInternal Medicine.
Among the PCP visits, the use of PSA testing declined from 36.5% in 2010 to 16.4% in 2012, for an odds ratio of 0.43 (95% CI, 0.23–0.81; P = .009). In contrast, the rate decreased among urologists from 38.7% only to 34.5%, for an odds ratio of 0.34 (95% CI, 0.10–1.20; P = .09). The authors noted that the difference between physician-specific testing practices was statistically significant (P < .001).
The difference in this decline, they wrote, “likely reflect opposing perceptions among physicians on the benefit of PSA screening,” as well as conflicting guidelines. For example, the American Urological Association recommends “shared decision-making” for men aged 55 to 69 years.
In an accompanying editor’s note, David S. Aaronson, MD, and Rita F. Redberg, MD, respectively of Kaiser Permanente and the University of California, San Francisco, wrote that “urologists may hold this belief because they have referred more men who request PSA testing or because they have seen more poor outcomes from metastatic prostate cancer.”
They noted that recommendations to reduce PSA screening will strengthen with the release of a National Committee for Quality Assurance measure aimed at eliminating PSA tests in men over 70 years of age. “Meanwhile, the widespread use of the PSA test should serve as a cautionary tale of the importance of first establishing that benefit exceeds harms before recommending new cancer screening tests,” they wrote.