Radiation Still Needed in Very Small, Node-Negative Invasive Breast Cancer
NEW ORLEANS-Preliminary results of National Surgical Adjuvant Breast and Bowel Project (NSABP) protocol B-21 have ended the “lingering, perhaps illusory hope of identifying a subset of women in whom radiation could be eliminated or replaced with another intervention” for treating early-stage invasive breast cancer, said Norman Wolmark, MD, chairman of the NSABP.
NEW ORLEANSPreliminary results of National Surgical Adjuvant Breast and Bowel Project (NSABP) protocol B-21 have ended the lingering, perhaps illusory hope of identifying a subset of women in whom radiation could be eliminated or replaced with another intervention for treating early-stage invasive breast cancer, said Norman Wolmark, MD, chairman of the NSABP.
Addressing the 36th ASCO meeting, Dr. Wolmark reported data comparing radiation plus placebo, radiation plus tamoxifen (Nolvadex), and tamoxifen alone in women with node-negative tumors of 1 cm or smaller who had lumpectomy and axillary lymph node dissection.
Tamoxifen cannot replace radiotherapy even in these favorable lesions, he stated. Data from NSABP show that the standard of care should remain unchanged, even for these small, very-favorable-risk cancers.
Surprising Differences
At a median follow-up of 68.3 months, cumulative 5-year risk of recurrence was over 10% with tamoxifen vs 4.8% with radiation plus placebo (P = .01). Cumulative 5-year risk with radiation plus tamoxifen was 2% vs 4.8% with radiation plus placebo (P = .0001). The magnitude of differences is somewhat surprising, Dr. Wolmark said. This is a big difference even for small tumors. Offering both therapies should become standard practice.
The NSABP trial enrolled 1,009 women, of whom 999 were evaluable. Five-year follow-up data were available for 73% of patients. Patients were randomized to tamoxifen alone (arm 1), radiotherapy plus placebo (arm 2), or radiotherapy plus tamoxifen (arm 3). Arms 2 and 3 were double-blinded.
The principal study objectives were to determine whether tamoxifen was as effective as radiotherapy in controlling ipsilateral breast tumor recurrence and whether the addition of tamoxifen to radiotherapy was superior to either modality alone.
Secondary endpoints included the effect of these treatments on disease-free survival and the occurrence of contralateral breast cancers.
Dr. Wolmark reported that the rate of ipsilateral recurrence [Table] was 2.8% with radiation plus tamoxifen vs 10.7% with tamoxifen alone (P = .0000002). The rate of ipsilateral recurrence was twofold greater in the group treated with tam-oxifen alone, compared to radiation alone (P = .009). Eighty percent of the ipsilateral recurrences were invasive.
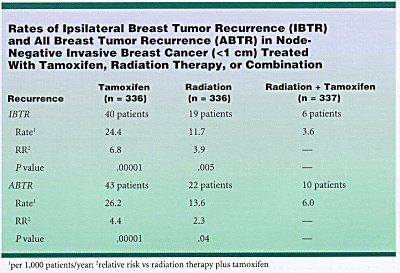
The rate of contralateral recurrence was 3.0% with radiation alone vs 0.6% with radiation plus tamoxifen (P = .04). Contralateral breast cancers occurred in 11 of 336 patients (3.3%) randomized to radiation alone and in 8 of 673 patients (1.2%) receiving tamoxifen (with or without radiation), a 65% reduction (P = .04).
There were no significant differences in overall or breast-cancer-related mortality in the three treatment groups.
Tamoxifen cannot replace radiation therapy for controlling ipsilateral breast cancer recurrences, and the combination of tamoxifen plus radiation therapy is superior to either therapy alone, Dr. Wolmark said.
He noted that tamoxifen also reduced the incidence of contralateral breast cancer, as it has in every other NSABP trial in which tamoxifen was tested.