Recently Approved ALL Drug Gets Big Price Tag
According to a report, two courses of the newly approved agent blinatumomab, for relapsed or refractory B-cell precursor ALL, will cost a staggering $178,000.
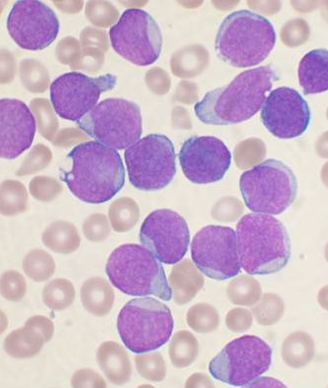
Bone marrow aspirate smear of precursor B-cell ALL; source: Dybdal, Wikimedia Commons
Two courses of the newly approved agent blinatumomab, used to treat relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL), will cost a staggering $178,000, according to an exclusive report by Reuters on Thursday.
The drug’s maker Amgen said the price reflects the significant value of the drug on an “ultra-orphan” population. Blinatumomab (Blincyto) was approved on December 3 by the US Food and Drug Administration, after an accelerated review process.
The approval was based on results from a phase II multicenter open-label study of 185 patients with Philadelphia chromosome-negative relapsed or refractory B-cell precursor ALL. Amgen called this a “rare and rapidly progressing cancer.” The trial found that 41.6% of patients achieved complete remission or complete remission with partial hematologic recovery within 2 cycles of blinatumomab therapy; the new pricing for 2 cycles reflects that trial endpoint. The majority of the responses seen (81%) actually occurred within the first treatment cycle.
Among only those patients who achieved a complete remission with hematologic recovery, 39% went on to receive hematopoietic stem cell transplantation, and 75.3% achieved minimal residual disease status.
The most common serious adverse events with blinatumomab included febrile neutropenia, pyrexia, pneumonia, and sepsis. The drug has a boxed warning in its labeling regarding the possibility of cytokine release syndrome, which can be life-threatening.
The high cost of the new agent could play a role in how it is used. One study from early in 2014 showed that higher copayments for chronic myeloid leukemia drugs make patients more likely to be non-adherent; those drugs, however, are generally intended to be taken for many years in a population that can often survive decades.
Another study, presented at the Palliative Care in Oncology Symposium in Boston in October, found that the financial burden of cancer treatment leads many to alter some aspect of lifestyle or the care itself. Thirty-nine percent of patients in the study took less medication than prescribed in order to defray the costs. Other recent research has shown that more than one quarter of cancer survivors report some financial problem.
The high cost of blinatumomab may reflect the limited patient population who could be eligible to take it. Reuters estimated that only about 1,000 American ALL patients would fit the eligibility requirements. If every single one of those patients took the drug in a given year, the company would earn $178 million. Amgen acquired the drug’s original developer Micromet in 2012 for $1.16 billion.