Recurrence Score Validated in Clear Cell RCC
A 16-gene Recurrence Score was found to be significantly predictive of recurrence-free interval and survival in patients with stage I-III clear cell renal cell carcinoma who have undergone nephrectomy.
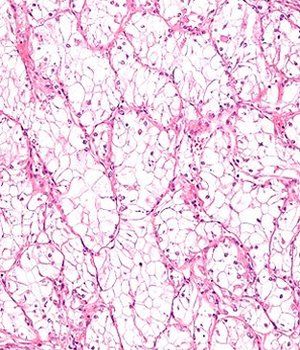
Intermediate magnification micrograph of a clear cell renal cell carcinoma; source: Nephron, Wikimedia Commons
A 16-gene Recurrence Score was found to be significantly predictive of recurrence-free interval and survival in patients with stage I-III clear cell renal cell carcinoma (RCC) who have undergone nephrectomy, according to data (abstract 4502) presented at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting.
“The Recurrence Score is able to identify a clinically relevant proportion of patients with stage I, II, and III [disease] with a very low risk of recurrence,” said study presenter Bernard J. Escudier, MD, of Institut Gustave Roussy, Villejuif, France. “Moreover, it identified a number of stage I patients with high risk of recurrence at 5 years.”
According to Escudier, in the future, this score may be useful for selecting patients for adjuvant treatment trials, for active surveillance of small renal masses, and for surveillance strategies after surgery.
Current evidence shows that about 30% of patients with localized clear cell RCC will relapse after surgery. Physicians are in need of prognostic markers that capture the underlying tumor biology and discriminate recurrence risk.
Escudier and colleagues conducted a prospective study using archived tissue designed to determine if there is a significant relationship between a prespecified Recurrence Score and risk for recurrence.
The Recurrence Score was developed in a Cleveland Clinic study where researchers looked at 732 genes selected from published data and biologic pathways that are functionally important to clear cell RCC. This list was then narrowed to 516 genes based on their associations with recurrence-free intervals. Next, 72 genes were selected based on the strength of their association with recurrence-free interval, key biological pathways, and having known drug targets. Finally, a panel of 16 genes was selected.
The researchers grouped these genes into those associated with better outcome (vascular and immune response genes) and those associated with worse outcome (cell growth/division and inflammation genes). The Recurrence Score was calculated with a formula that took into account the weight and importance of each group of genes, with genes associated with better outcomes getting a negative score and those associated with a worse outcome getting a higher score; the Score was scaled from 0 to 100.
Escudier and colleagues then evaluated the clinical utility of the score in 622 patients.
Results of the study showed that stage and grade of tumor were highly prognostic. The risk of recurrence was 7% for stage I, 16% for stage II, and 30% for stage III. Similarly, the risk for recurrence was 0% for grade 1, 6% for grade 2, 15% for grade 3, and 30% for grade 4 tumors.
Results of the primary analysis showed that for each 25-unit increase in the Recurrence Score, the risk for recurrence increased almost fourfold (HR = 3.9; 95% CI, 2.6-5.8; P < .001). Even after adjustment in multivariable analysis, the Recurrence Score remained predictive with a hazard ratio per 25 unit score increase of 3.4 (95% CI, 2.2-5.1; P < .001).
In addition, the Recurrence Score predicted renal cancer specific survival, disease-free survival, and overall survival.
The researchers were also able to use the Recurrence Score to further stratify patients by recurrence risk in stage I and stage II-III patients. Among patients with stage I disease, those with a low score (< 32) had a 5-year risk for recurrence of 2%; intermediate score, 8%; and high score (45 or higher), 23%. The same was true for patients with stages II-III disease with a low score, 2%; intermediate score, 26%; and high score, 39%.