Regorafenib Improves PFS in Non-Adipocytic Soft-Tissue Sarcoma
A phase II trial found that the multikinase inhibitor regorafenib has clinical activity and offers improved progression-free survival in certain types of advanced soft-tissue sarcoma.
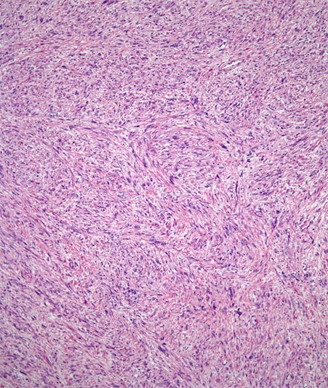
Low-power view of a leiomyosarcoma
A phase II trial found that the multikinase inhibitor regorafenib has clinical activity and offers improved progression-free survival (PFS) in certain types of advanced soft-tissue sarcoma (STS).
“Despite primary combined modality therapy, at least 40% of [STS] patients develop recurrent or metastatic disease,” wrote study authors led by Olivier Mir, MD, of Institut Gustave Roussy in Villejuif, France. There are some approved treatment options for advanced STS patients, but overall survival remains poor. Pazopanib, a VEGFR2 and angiogenesis inhibitor, has been shown to improve PFS, but not overall survival, and further options are still needed.
The new trial tested regorafenib, which has activity against VEGFR1, 2, and 3, as well as several tumor cell signaling kinases, in 182 STS patients. Patients were separated by sarcoma subtype (43 liposarcoma patients, 56 leiomyosarcomas, 27 synovial sarcomas, and 56 other sarcoma types) and randomized to either regorafenib or placebo. The results were published online ahead of print in Lancet Oncology.
In the liposarcoma cohort, the median PFS was 1.1 month with regorafenib and 1.7 months with placebo, for a hazard ratio (HR) of 0.89 (95% CI, 0.48–1.64; P = .70). The other three cohorts did see a PFS benefit with the study drug, however.
The median PFS in leiomyosarcoma patients was 3.7 months with regorafenib and 1.8 months with placebo, for an HR of 0.456 (95% CI, 0.26–0.80; P = .0045). In synovial sarcoma patients, these rates were 5.6 months and 1 month, respectively, for an HR of 0.10 (95% CI, 0.03–0.35; P < .0001). Finally, the other sarcoma patients had a PFS of 2.9 months with regorafenib and 1 month with placebo, for an HR of 0.46 (95% CI, 0.25–0.82; P = .0061).
Though the differences did not reach significance, there was numerical improvement in overall survival in the latter three sarcoma subtypes as well. The median overall survival was worse with regorafenib than placebo in the liposarcoma cohort.
The researchers conducted an unplanned pooled analysis of the non-adipocytic sarcomas. The median PFS was 4 months in these patients with regorafenib, compared with 1 month with placebo, for an HR of 0.36 (95% CI, 0.25–0.53; P < .0001). The median overall survival was 13.4 months with the study drug, and 9 months for placebo, for an HR of 0.67 (95% CI, 0.44–1.01; P = .059).
The most common clinically significant adverse events were arterial hypertension, in 19% of regorafenib patients and only 2% of placebo patients; hand and foot skin reaction in 15% vs 0%; and asthenia in 13% vs 6% of patients. One patient treated with regorafenib died due to hepatitis-induced liver failure, and this was determined to be treatment-related.
“We showed that patients with advanced non-adipocytic [STS] previously treated with anthracycline-based chemotherapy had longer [PFS] when treated with regorafenib compared to patients treated with placebo,” the authors concluded. “Further clinical trials are warranted.”
Sarcoma Awareness Month 2023 with Brian Van Tine, MD, PhD
August 1st 2023Brian Van Tine, MD, PhD, speaks about several agents and combination regimens that are currently under investigation in the sarcoma space, and potential next steps in research including immunotherapies and vaccine-based treatments.