Relugolix Demonstrates Efficacy Regardless of Baseline Testosterone Levels in Advanced Prostate Cancer
Patients with advanced prostate cancer benefitted from relugolix vs leuprolide regardless of baseline testosterone level.
Relugolix yielded positive safety and efficacy in advanced prostate cancer across all baseline testosterone levels, according to data from a subgroup analysis of the phase 3 HERO trial (NCT03085095) that were presented at the Society for Urologic Oncology (SUO) 23rd Annual Meeting.
In the population of 912 patients who had their baseline testosterone collected during the trial, a total of 147 patients—including 96 in the relugolix arm and 51 in the leuprolide arm—had a baseline level of less than 280 ng/dL—and 765—including 516 in the relugolix arm and 249 in the leuprolide arm—had a level of 280 ng/dL. Although the population had advanced age, most patients had testosterone levels that were within a normal range.
“The outcomes were similar between [patients with advanced prostate cancer] who had normal or above, or below normal testosterone levels at baseline,” said the lead study author in an interview with CancerNetwork®. “There’s a thought that patients who come in with lower levels of testosterone may have worse outcomes, so we wanted to look at the ability to sustain castration in those 2 groups. It ended being that relugolix was effective in both groups.”
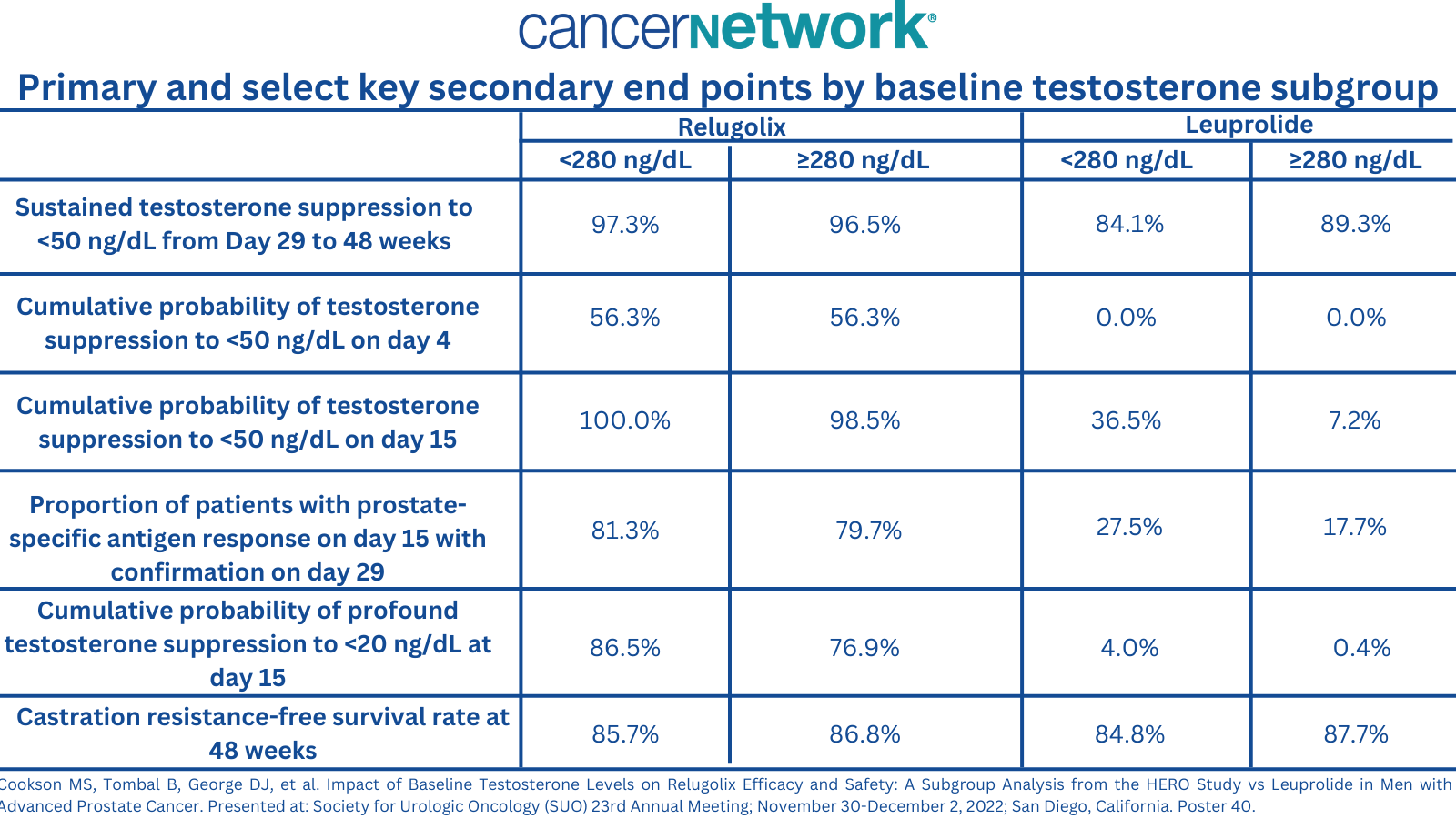
The 48-week point estimated castration rates were notably higher among patients treated with relugolix vs leuprolide in each respective subgroup. In the relugolix arm, patients with a level of less than 280 ng/dL and 280 ng/dL or more had rates of 97.3% and 96.5%, respectively, vs 84.1% and 89.3% in the leuprolide arm. The sustained castration rates were 96.7% and 88.8% in the overall population, respectively.
“Relugolix in men regardless of their baseline testosterone level showed equal efficacy,” according to Kelly L. Stratton, MD, an assistant professor of urologic oncology in the Department of Urology and an adjunct assistant professor of medical oncology at the Stephenson Cancer Center at Ohio University Health, in an interview with CancerNetwork®. “The outcomes were similar between those who had normal or above, or below normal testosterone levels at baseline. There’s a thought that patients who come in with lower levels of testosterone may have worse outcomes, so we wanted to look at the ability to sustain castration in those 2 groups. It ended being that relugolix was effective in both groups.”
The HERO trial included a total of 930 patients with advanced prostate cancer who were randomly assigned 2:1 to receive either relugolix at a dose of 120 mg daily following a single loading dose of 360 mg or a 3-month leuprolide injection for 48 weeks.
Patients who had a baseline testosterone level of less than 280 ng/dL or 280 ng/dL or higher were assessed in the subgroup analysis and included assessment of sustained testosterone suppression to castrate levels from day 29 to 48 weeks, early castration rates, prostate-specific antigen (PSA) levels, castration resistance-free survival (CRFS) at 48 weeks, and safety.
In the relugolix arm, 68.8% and 71.9% of patients in the low and high testosterone cohorts were 75 years or younger, respectively, with a median age of 72 years.
The median PSA level in each respective cohort was 11.1 ng/mL and 11.8 ng/mL and the mean testosterone level was 228.5 ng/dL and 474.7 ng/dL, respectively. Additionally, most patients had metastatic disease at study entry (32.3% and 31.8%, respectively) followed by locally advanced disease (29.2% and 30.8%), and localized disease (29.2% and 28.3%).
In the leuprolide cohort, patients had median ages of 70 years and 71 years in the low and high testosterone groups, respectively, and 76.5% and 71.1% of patients were 75 years and younger. The median PSA was 12.5 ng/mL and 8.9 ng/mL in each respective group, and the mean testosterone levels were 227.6 ng/dL and447.3 ng/dL, respectively.
This cohort primarily had metastatic disease (37.3% and 30.9%, respectively) followed by locally advanced disease (27.5% and 30.9%), and localized disease (25.5% and 11.2%).
Key secondary end points also appeared to favor those treated with relugolix vs leuprolide with the exception of CRFS, which was similar between treatment groups and subgroups.
Primary and select key secondary end points by baseline testosterone subgroup from a subgroup analysis of the phase 3 HERO trial (NCT03085095).
In the relugolix cohort, 24.0% of patients with a low testosterone level had grade 3 or higher adverse events (AEs), compared with 17.2% of those with a high level. Moreover, serious AEs occurred in 16.7% and 11.4% and fatal AEs occurred in 2.1% and 1.0%, respectively. The most common any grade AEs in each respective group included hot flash (52.1% and 54.8%, respectively), fatigue (30.2% and 20.2%), and diarrhea (14.6% and 11.6%).
The low-level testosterone group had 2 events of grade 3 or higher hypertension while the high-level group had 8 events of hypertension and 4 events of hot flash.
In the leuprolide group, 21.7% of patients in the low testosterone group had high-grade AEs, compared with 20.5% in the high-level group. Moreover, 17.6% and 15.3% of patients, respectively, had serious AEs and 5.9% and 2.4% had fatal AEs.
Common any grade AEs in this population included hot flash (56.9% and 51.8%, respectively), hypertension (27.5% and 8.4%), and fatigue (15.7% and 19.7%), with 1 event each of high-grade hypertension and 3 events of backpain.
Reference
Cookson MS, Tombal B, George DJ, et al. Impact of Baseline Testosterone Levels on Relugolix Efficacy and Safety: A Subgroup Analysis from the HERO Study vs Leuprolide in Men with Advanced Prostate Cancer. Presented at: Society for Urologic Oncology (SUO) 23rd Annual Meeting; November 30-December 2, 2022; San Diego, California. Poster 40.