Ribociclib Combo Yields Survival Benefits in HR+/HER2– Breast Cancer
Combining ribociclib with endocrine therapy appears to be effective and tolerable for those with hormone receptor–positive HER2-negative advanced breast cancer, including elderly patients.
“Analysis showed that [ribociclib plus endocrine therapy] is an effective and well-tolerated treatment in general,” according to Lowell Hart, MD, FACP.
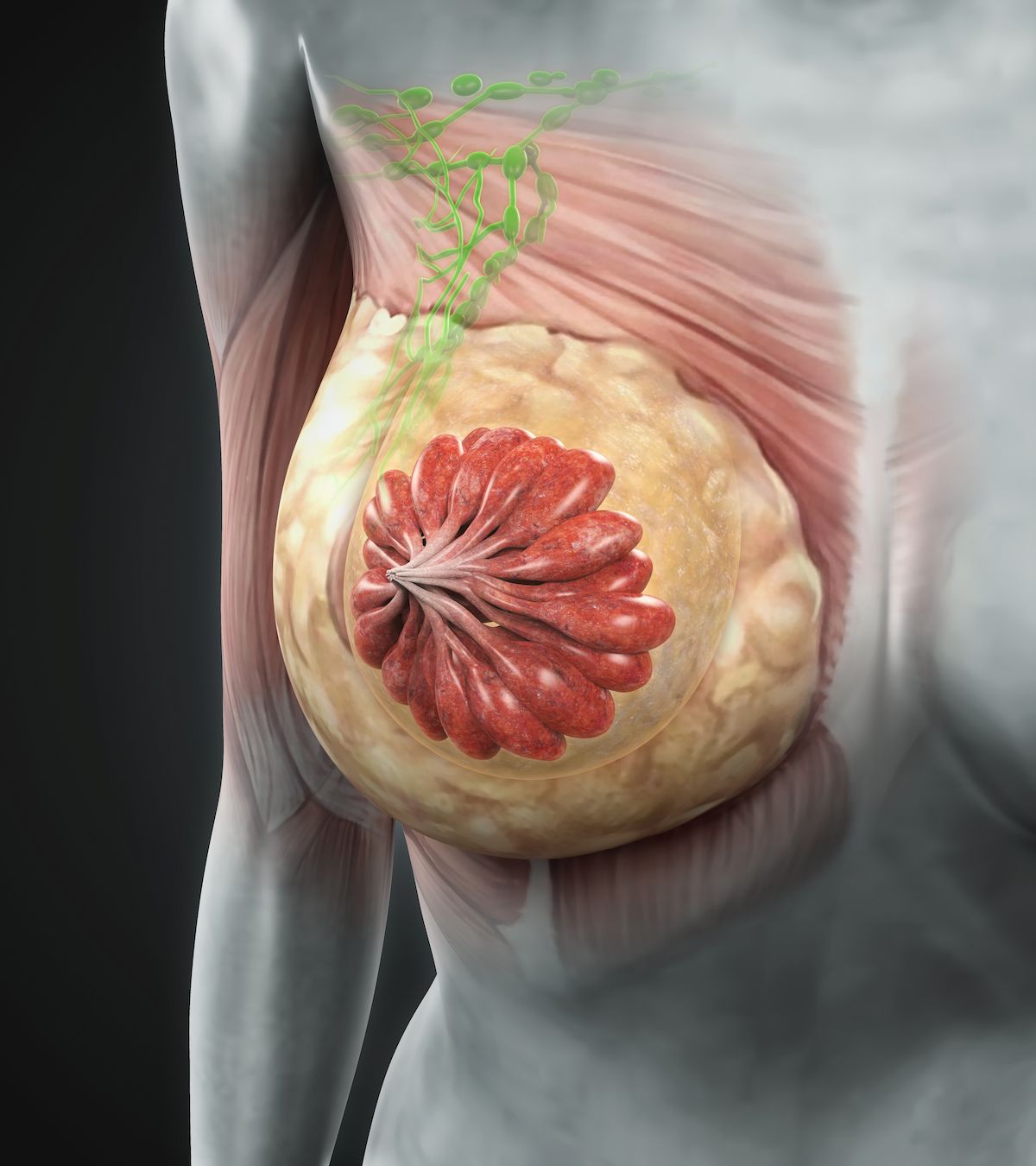
Treatment with ribociclib (Kisqali) plus endocrine therapy produced consistent progression-free survival (PFS) and overall survival (OS) benefits compared with placebo plus endocrine therapy among patients with hormone receptor (HR)–positive HER2-negative advanced breast cancer regardless of age, according to findings from an analysis of the MONALEESA trials presented at the 2023 San Antonio Breast Cancer Symposium (SABCS).1
Investigators reported a median PFS of 31.8 months with the ribociclib combination vs 16.4 months with placebo plus endocrine therapy in patients younger than 65 years (HR, 0.56; 95% CI, 0.47-0.66). Additionally, the median PFS in each respective arm was 35.7 months vs 19.2 months in patients 65 years and older but younger than 75 (HR, 0.55; 95% CI, 0.42-0.73) and 31.1 months vs 19.2 months in those 75 years or older (HR, 0.54; 95% CI, 0.34-0.86).
Among patients younger than 65 years, the median OS was 67.6 months in the ribociclib arm vs 51.7 months in the placebo arm (HR, 0.69; 95% CI, 0.56-0.84). The median OS in each respective arm was 72.6 months vs 59.8 months in patients 65 years and older but younger than 75 (HR, 0.79; 95% CI, 0.58-1.07) and 62.1 months vs 52.8 months in those 75 years and older (HR, 0.75; 95% CI, 0.46-1.21).
The median time to next chemotherapy (TTC) in patients younger than 65 years was 58.0 months in the ribociclib arm compared with 40.2 months in the placebo arm (HR, 0.67; 95% CI, 0.55-0.83). Additionally, the median TTC in each respective arm was not evaluable and 48.3 months in patients 65 years and older but younger than 75 (HR, 0.64; 95% CI, 0.47-0.89) and 80.3 months vs 42.3 months in patients 75 years and older (HR, 0.48; 95% CI, 0.27-0.87).
“Analysis showed that [ribociclib plus endocrine therapy] is an effective and well-tolerated treatment in general,” presenting author Lowell Hart, MD, FACP, a medical oncologist and hematologist at Florida Cancer Specialists & Research Institute in Fort Myers, Florida, and an associate professor at Wake Forest University School of Medicine in Winston-Salem, North Carolina, said. “We didn’t see any unusual [adverse] effects [AEs] in the more elderly patients.”
Investigators of this pooled data analysis evaluated outcomes among patients who are postmenopausal in the phase 3 MONALEESA-2 trial (NCT01958021)2 and phase 3 MONALEESA-3 trial (NCT02422615)3 as well as patients who were premenopausal in the phase 3 MONALEESA-7 trial (NCT02278120).4 The median follow-up for the MONALEESA-2, MONALEESA-3, and MONALEESA-7 trials, respectively, was 79.8 months, 70.8 months, and 54.4 months.
In the MONALEESA-2 trial, 668 patients were randomly assigned 1:1 to receive ribociclib at 600 mg orally once a day or a matched placebo in a 3-weeks-on and 1-week-off schedule followed by letrozole (Femara) at 2.5 mg per day. In the MONALEESA-3 trial, 726 patients were randomly assigned 2:1 to receive ribociclib or a matched placebo at 600 mg/day for 3 weeks on and 1 week off followed by 500 mg of fulvestrant. The MONALEESA-7 trial included 672 patients who were randomly assigned 1:1 to receive ribociclib or placebo at 600 mg/day for 3 weeks on and 1 week off followed by tamoxifen or a nonsteroidal aromatase inhibitor plus goserelin.
Investigators of this exploratory analysis assessed PFS, OS, and TTC across patient age groups based on Kaplan-Meier methodology. The analysis also evaluated patient-reported outcomes based on responses to the European Organization for Research and Treatment of Cancer QLQ-C30 (EORTC-QLQ C30). Additionally, investigators assessed the time to definitive deterioration (TTD) in global health status and change in physical functioning.
The overall population in the pooled dataset included 1229 patients. Of these patients, 773 were younger than 75 years and 456 were older than 65 years. Investigators reported that baseline characteristics were comparable across age groups in each treatment arm, although they noted a few key differences. In the ribociclib and placebo arms, respectively, there was a higher proportion of patients in the 75 years and older group with an ECOG performance status of 1 (46% and 49%) compared with patients in the younger than 65 (31% and 31%) and 65 years and older but younger than 75 (46% and 39%) groups. Moreover, more patients in the younger than 65 group had de novo disease (43% and 43%) compared with those 65 years and older but younger than 75 (38% and 37%) and 75 years and older groups (38% and 36%).
Across each treatment arm and patient age group, anywhere from 73% to 90% of patients received any subsequent therapy. Endocrine therapy alone was the most common subsequent treatment for patients in the ribociclib arm across all age groups. The most common first subsequent therapy in the placebo arm was any chemotherapy in all age groups except the 65 years and older but younger than 75 group, in which the most frequent subsequent therapy was endocrine therapy alone.
The incidence of AEs and AEs of special interest were comparable across all patient subgroups and were typically manageable with standard dose modifications. Common any-grade AEs of special interest included neutropenia in 63% to 79% of patients who received ribociclib and 4% to 8% of those who received placebo.
In the ribociclib and placebo arms, respectively, the highest treatment discontinuation following AE rates were observed in the 75 years and older group (41% vs 8%). Treatment discontinuation in the experimental arm was generally the result of liver enzyme level increases. The rate of patients who discontinued treatment in the ribociclib arm due to AEs without prior dose reduction was 34% in the younger than 65 years group, 41% in the 65 and older but younger than 75 group, and 50% in the 75 and older group.
The experimental regimen yielded a TTD benefit across all age groups with respect to pain score and fatigue score. TTD was comparable between treatment arms in the 75 years and older group with respect to global health status and physical functioning; a more notable benefit in these outcomes with the ribociclib combination occurred in the other age groups.
References
- Hart L, Im S, Tolaney SM, et al. Efficacy, safety, and quality of life with ribociclib + endocrine therapy in elderly patients with HR+/HER2– advanced breast cancer across the MONALEESA-2, -3, and -7 trials. Presented at the 2023 San Antonio Breast Cancer Symposium; December 5-9, 2023; San Antonio, TX; abstract PS02-01.
- Hortobagyi GN, Stemmer SM, Burris HA, et al. Overall survival with ribociclib plus letrozole in advanced breast cancer. N Engl J Med. 2022;386:942-950. doi:10.1056/NEJMoa2114663
- Slamon DJ, Neven P, Chia S, et al. Overall survival with ribociclib plus fulvestrant in advanced breast cancer. N Engl J Med. 2020;382:514-524. doi:10.1056/NEJMoa1911149
- Im S, Lu Y, Bardia A, et al. Overall survival with ribociclib plus endocrine therapy in breast cancer. N Engl J Med. 2019;381:307-316. doi:10.1056/NEJMoa1903765