Right Age for Lynch Syndrome Screening Still in Question
The results of a recent meta-analysis suggest that carriers of the MLH1 or MSH2 mutations associated with Lynch syndrome could delay regular colonoscopies until age 30.
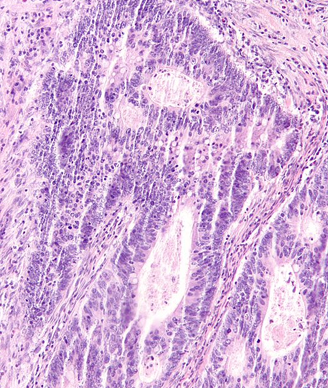
High magnification micrograph of tumor infiltrating lymphocytes (TILs) in a case of colorectal carcinoma. TILs are associated with microsatellite instability cancers, as seen in Lynch syndrome. Copyright 2012 Nephron.
People with a familial history of Lynch Syndrome are currently advised to undergo colonoscopy screening for colorectal cancer every 1 to 2 years regardless of age or sex, however, the results of a recent meta-analysis published in the Journal of Clinical Oncology, suggest that carriers of the MLH1 or MSH2 mutations associated with Lynch Syndrome could delay regular colonoscopies until age 30.
Mark A. Jenkins, PhD, of the University of Melbourne, and colleagues found for people in their 20s that on average 1 in 71 men and 1 in 102 women with MLH1 or MSH2 mutations will be diagnosed with colorectal cancer in the next 5 years. This equated to 1 death prevented and 1 serious complication occurring for every 155 men or 217 women in their 20s who underwent annual screening.
To get these data, the researchers looked at pooled estimates from all independent published Lynch syndrome studies reporting age- and sex-dependent colorectal cancer risk. The studies included 1,114 families.
“Five-year risks increased from approximately 1% for mutation carriers in their 20s (roughly equivalent to that for a noncarrier who is 60 years older) to 9% to 14% for mutation carriers in their 50s, and then decreased to 5% to 8% for mutation carriers in their 70s,” the researchers wrote. “The reason for the initial increase and then decrease of risk for carriers with age is a result of the initially rapid and then more tempered decrease of hazard ratio with age for carriers against the exponentially increasing colorectal cancer risk with age for the general population.”
Specifically, the data showed that risk for colorectal cancer peaked in people in their 50s with, on average, 1 in 7 men and 1 in 12 women who had MLH1 or MSH2 mutations being diagnosed with colorectal cancer over 5 years. By their 70s, the average rate for diagnosis of colorectal cancer was 1 in 13 men and 1 in 19 women.
For people in their 50s, annual colonoscopy in 16 men or 25 women would prevent 1 death from colorectal cancer over 5 years, with “almost no serious complications,” the researchers reported.
“Annual colonoscopy for those older than age 30 years seems warranted, but screening of carriers in their 20s might not be justifiable given the large number of colonoscopy procedures required to prevent one death from colorectal cancer,” the researchers wrote.
However, in an editorial that accompanied the meta-analysis, Molly S. Daniels, MS, CGC, and Karen H. Lu, of the University of Texas MD Anderson Cancer Center wrote, “Setting the age at which to begin cancer screening is challenging when occasional cancers occur in younger patients. Given that 6 of 367 colorectal cancers in this study were diagnosed before age 30 years, is deferring colonoscopy until age 30 years appropriate? Given the lack of consensus on how to choose this cutoff, we would recommend considering family history and patient preference in deciding when to begin colorectal cancer screening.”