Risk Model Effectively Predicts pN2b Metastasis in N2-suspected NSCLC
Investigators developed a risk model to assess whether upfront surgery can improve prognoses in a subset of cN2 diseases such as single-station N2 NSCLC.
Investigators developed a risk model to assess whether upfront surgery can improve prognoses in a subset of cN2 diseases such as single-station N2 NSCLC.
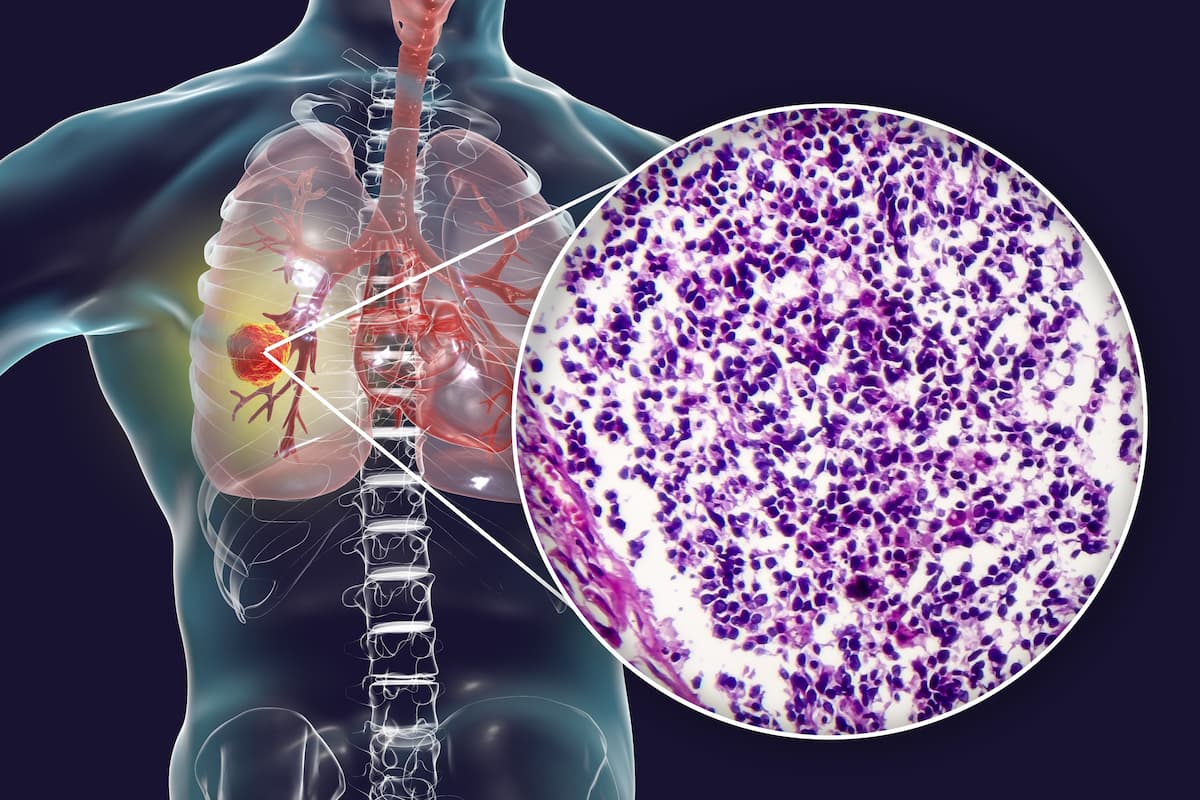
A risk model developed with preoperative clinical variables effectively predicted pathological multi-station N2 (pN2b) metastasis in patients who underwent upfront surgery for suspected clinical single-station N2 (cN2a) non–small cell lung cancer (NSCLC), according to findings from a study published in Scientific Reports.The risk model was developed to assess whether upfront surgery can improve prognosis in a subset of cN2 diseases, including cN2a NSCLC.
Data showed an advantage in 5-year overall survival (OS) rates for pN2a1 (51.1%) and pN2a2 disease (45.8%) over pN2b disease (29.0%; P = .041). Additionally, the risk scoring system based on the model showed discriminant ability for pN2b disease (area under receiver operating characteristic [AUROC], 0.779). Furthermore, independent risk factors for pN2b metastasis included histologic type (p <.001), age of 50 years or younger (p <.001), preoperatively confirmed N2 metastasis (p <.001), and clinical stage IIIB as opposed to IIIA (p = .003).
The total 5-year OS rate was 49.2%, with a 5-year recurrence-free survival (RFS) rate of 44.5%. Additionally, 5-year OS rates for cIIIA and cIIIB were 52.5% and 43% (P = .04), and RFS rates were 50.5% and 36%, respectively (P = .001). Similar to OS rates, observed differences between pN2a1, pN2a2, and pN2b in RFS were significant (P = 0.03).
“According to our results, patients with pN2b had a significantly poorer prognosis than those with pN2a1 and pN2a2, even in some patients with cN2a NSCLC. Using preoperative clinical variables, we developed a risk-scoring system for predicting the probability of multiple N2 metastasis in patients with cN2a, which showed excellent discriminant ability [AUROC: 0.773],” Jae Kwang Yun, MD, professor at the Department of Thoracic and Cardiovascular Surgery at the Asan Medical Center in the Ulsan University College of Medicine in Seoul, South Korea, wrote with study coinvestigators in the publication. “To the best of our knowledge, this scoring system is the first to present a risk model for postoperative pN2b among [patients with] cN2a [disease], using a sufficient number of patients at a single institution.”
Clinical records were retrospectively collected for patients who underwent surgery for NSCLC in the Thoracic Surgery Department at Asan Medical Center in Seoul, South Korea between 2006 and 2018 (n = 961). Among patients who were evaluated, through use of image modalities such as chest CT or PET-CT, single-station N2 node metastasis was clinically suspected in 547.
CN2a disease was defined as enlarged lymph node of 10 mm or greater on the largest short axis on chest CT or PET-positive lymph nodes in single N2 node. Upfront surgery was considered if the primary tumor could be resected without the need for pneumonectomy, the involved lymph nodes were distinct from surrounding tissue and less than 3.0 cm, and CT or PET scans showed no extra-nodal tumor invasion.
Adjuvant chemotherapy was recommended for patients with pN2 disease younger than 75 and in better than poor physical condition. Systemic adjuvant chemotherapy with a platinum-based regimen was recommended with 4 cycles postoperatively over 4 to 6 weeks. Total dosage for adjuvant radiotherapy reached 50.4 Gy and 55 to 60 Gy for patients with complete resection or positive resection margins, respectively, at 1.8 Gy daily.
Follow-up data was collected every 3 months for the first 2 years following surgery, every 6 months for the next 3 years, and then annually. As part of routine follow-up, chest CT was performed, with PET-CT performed with clinical suspicion of disease recurrence.
Of 547 patients with cN2a NSCLC, pathological staging was pN0 and pN1 following surgery in 176. There were 77, 165, and 165 patients with pN2a1, pN2a1, and pN2b disease, respectively, among patients with pN2 disease.
Reference
Kim JY, Lee HP, Yun JK, et al. Risk prediction of multiple-station N2 metastasis in patients with upfront surgery for clinical single-station N2 non-small cell lung cancer. Sci Rep. 2024;14:18800. doi:10.1038/s41598-024-69260-3