RNA Test for HPV Helps Stratify Cervical Cancer Risk
A test for dangerous strains of high-risk HPV using messenger RNA was shown to be reliable and effective for cervical cancer risk stratification.
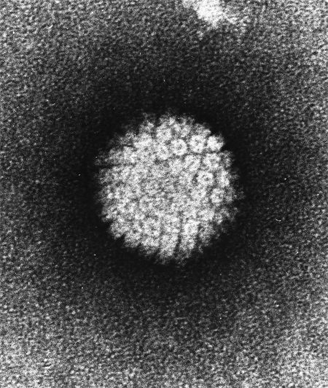
Electron micrograph of a negatively stained HPV
A test for several dangerous strains of high-risk human papillomavirus (HPV) using messenger RNA was shown to be reliable and effective for cervical cancer risk stratification among women with atypical results of a Papanicolaou (Pap) test, according to the results of a new study.
Results from the CLEAR study previously led to US Food and Drug Administration of approval of the Aptima genotype assay (Hologic) in October 2012. “High-risk human papillomavirus testing is now recommended for use with Pap testing for routine cervical cancer screening and for the management of women with atypical squamous cells of undetermined significance Pap results,” wrote study authors led by Damon Getman, PhD, of Hologic (the company also funded the CLEAR trial). This new analysis reflex tested women with a positive Aptima test using a specific HPV 16 18/45 genotype assay (AHPV-GT) for further stratification.
The study included 912 women with atypical squamous cells of undetermined significance on a Pap test, and the AHPV-GT test was performed on those found to be positive for high-risk HPV. Of that total, 893 (97.9%) received a definitive diagnosis with AHPV-GT testing.
In the full cohort, 38.8% were high-risk HPV positive; this rate decreased in ascending age groups, from 57% for those aged 21 to 29 years down to 16.7% in those aged 40 years and older (P < .001 for trend). Among the high-risk HPV-positive women, 32.7% of the younger group were positive on the AHPV-GT assay, compared with 37.1% for 30- to 39-year-olds and 35.6% for those at least 40 years of age. AHPV-GT-positive women in the younger group were more likely to be HPV 16-positive, which is most strongly associated with cervical cancer. Women 30 years or older were more likely to be HPV 18/45-positive.
The risk of subsequent detection of cervical intraepithelial neoplasia grade 2 or more (CIN2+) was highest among HPV 16-positive women, at 37%. The risk was 15.9% for HPV 18/45-positive individuals, 14.3% for other high-risk HPV positives, and only 2.2% for AHPV-GT-negative women. Grade 3 (CIN3) or adenocarcinoma in situ was found in 20.5% of HPV 16-positive women, 9.1% of HPV 18/45-positives, 4.3% of other high-risk HPV-positive individuals, and only 0.7% of HPV-negatives.
“It will be critical to introduce new, more specific biomarkers or algorithms to minimize the harms of screening in… lower risk populations,” the authors wrote. “Second, these results raise the question of whether some of these women, especially younger women who are still intending to have children, might benefit from clinical management involving repeat testing in a year rather than being referred to colposcopy.” They concluded that these results show the AHPV-GT test to be an effective risk stratification method for women with abnormal Pap test results.