Robot-Assisted Prostate Cancer Surgery on the Rise
The adoption of robot-assisted radical prostatectomy is on the rise in the United States, according to the results of a retrospective study.
From 2003 to 2010 there has been a huge uptick in robot-assisted radical prostatectomies.
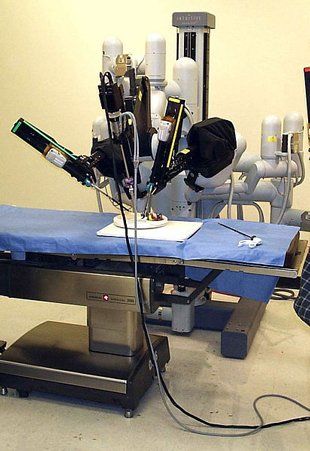
The adoption of robot-assisted radical prostatectomy (RARP) is on the rise in the United States, according to results of a retrospective study. Between 2003 and 2010, surgeons performing radical prostatectomies increased from 0.7% to 42%. The procedure is now widely available in the United States. The study is published in BJU International.
The cost of prostate cancer surgery at hospitals from 2003 to 2010 increased from $500 million annually to $700 million. Robotic-assisted surgery costs more than traditional surgery, accounting for a large portion of the 40% increase in yearly prostate cancer surgery expenses. However, median RARP costs decreased and leveled off during the course of the study at just above $10,000, while the cost of traditional radical prostatectomies increased to almost $9,000 by the end of 2010.
High-volume surgeons, who perform more than 24 radical prostatectomies per year, were more likely to adopt RARP. Surgeons at high-volume centers and teaching hospitals, as well as intermediate- and large-sized hospitals were also more likely to adopt RARP.
Steven L. Chang, MD, MS, of the division of urology at the Dana-Farber Cancer Institute, and colleagues analyzed a cohort of 489,369 men who had either open or laparoscopic radical prostatectomy or RARP between 2003 and 2010. The cohort data came from a national database, the Premier Hospital Database, which tracks about 20% of inpatient care in the United States. RARP adoption was defined as more than 50% of total radical prostatectomies in a given year.
The first robotic surgical system for use in urologic surgery was approved by the US Food and Drug Administration (FDA) in 2000, and the system was applied to prostatectomy procedures by 2001.
According to the study, there was a ramp up in the adoption rate, with the majority of uptake occurring between 2007 and 2010.
From 2003 to 2010, the number of surgeons in the United States performing radical prostatectomies decreased from about 10,000 to 8,200. But RARP adoption led to a larger volume of prostatectomies performed per surgeon as the drop off was mostly seen in the number of low-volume surgeons. The number of high-volume surgeons rose from 2% to 7%, and the number of radical prostatectomies they performed increased from 10% to 45%.
“Our study surprisingly found that the median cost of non-robot-assisted radical prostatectomy (open radical prostatectomy) has incrementally increased over time. We suspect that this is because the highest volume surgeons have largely shifted away from this surgical approach,” Chang told Cancer Network. The gradual decrease in the cost of robot-assisted radical prostatectomy, the authors suspect, is due to the preferential adoption of this technique by the same high-volume surgeons who likely have greater efficiency and reduced costs.
The authors conclude that adoption of RARP has likely stabilized in the United States since the majority of high-volume surgeons have already adapted a robotic system by 2010 and because not many intermediate-volume surgeons will likely invest in the robotic technique.
“Indirectly, we feel that the financial and time investments necessary to perform this procedure may have resulted in centralization of prostate surgery to higher volume surgeons and institutions, which may improve the overall care of men with prostate cancer,” said Chang.
For more on the use of robot-assisted radical prostatectomy, the editors suggest a Pro/Con from the journal ONCOLOGY.
Current Status of Robot-Assisted Radical Prostatectomy: Progress Is InevitableVipul R. Patel, MD, and Ananthakrishnan Sivaraman, MS
Minimally Invasive Open Retropubic Prostatectomy: In Experienced Hands-Still the Gold StandardJudd W. Moul, MD, FACS