Sacituzumab Govitecan/Pembrolizumab Yields Significant PFS Improvement in TNBC
Sacituzumab govitecan plus pembrolizumab showed a trend for improved overall survival vs standard of care in patients with untreated PD-L1–positive TNBC.
The safety profile of sacituzumab govitecan plus pembrolizumab was consistent with the safety profile for each individual agent, and no new safety signals were identified.
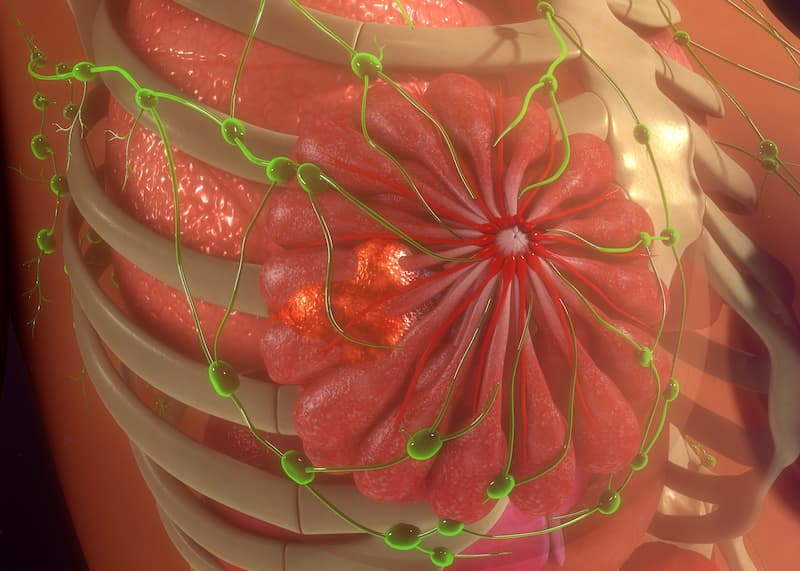
Sacituzumab govitecan-hziy (Trodelvy) in combination with pembrolizumab (Keytruda) had a statistically significant and clinically meaningful progression-free survival (PFS) outcome vs pembrolizumab plus chemotherapy in patients with unresectable, locally advanced or metastatic triple-negative breast cancer (TNBC) with PD-L1 expression who had a combined positive score of 10 or more, according to a news release from the drug’s developer, Gilead Sciences, Inc.1
Data from the phase 3 ASCENT-04/KEYNOTE-D19 trial (NCT05382286) revealed that the primary end point of PFS was met. Additionally, although overall survival (OS), a key secondary end point, was not mature at the time of data cutoff, an early trend for improved OS was observed with the investigational regimen vs pembrolizumab/chemotherapy.
Furthermore, the safety profile of sacituzumab govitecan plus pembrolizumab was consistent with the safety profile for each individual agent and no new safety signals were identified.
“For patients with metastatic [TNBC], there is a critical need for more effective treatment options,” Sara Tolaney, MD, MPH, associate professor of medicine at Harvard Medical School, chief of the Division of Breast Oncology at the Dana-Farber Cancer Institute, and primary investigator of the ASCENT-04 study, stated in the news release on the PFS analysis.1 “These data suggest that the combination of sacituzumab govitecan and pembrolizumab may offer a new treatment approach, bringing together a potent antibody-drug conjugate with immunotherapy to improve outcomes for patients.”
Patients in the phase 3 ASCENT-04 study were randomly assigned 1:1 to receive sacituzumab govitecan/pembrolizumab or pembrolizumab plus a chemotherapy agent of the physician’s choice.2 Those in the experimental arm received 10 mg/kg of sacituzumab govitecan on days 1 and 8 and 200 mg of intravenous pembrolizumab on day 1 of 21-day cycles for a maximum of 35 cycles.
In the active comparator arm, patients received 200 mg of pembrolizumab on day 1 of 21-day cycles plus chemotherapy of physician’s choice. Chemotherapy consisted of either 90 mg/m2 of paclitaxel on days 1, 8, and 15 of 28-day cycles; 100 mg/m2 of nab-paclitaxel on days 1, 8, and 15 of 28-day cycles; or 1000 mg/m2 of gemcitabine plus carboplatin area under the curve 2 on days 1 and 8 of 21-day cycles. Treatment persisted until disease progression or unacceptable toxicity verified by blinded independent central review, and patients assigned to chemotherapy were permitted to cross over to receive sacituzumab govitecan following disease progression.
In addition to OS, secondary study end points included objective response rate, duration of response, and time to deterioration in health-related quality of life.
Sacituzumab govitecan is a Category 1 preferred treatment for patients with metastatic TNBC as a second-line treatment or later and pretreated hormone receptor–positive/HER2-negative metastatic breast cancer per the NCCN Clinical Practice Guidelines in Oncology.3
Results from the study will be presented at a future medical meeting and discussed with regulatory authorities, and the safety and efficacy of sacituzumab govitecan in patients with untreated PD-L1–positive metastatic TNBC have not been previously established.
To be eligible for enrollment, patients with untreated PD-L1–positive locally advanced, inoperable, or metastatic TNBC must have treatment for stage I to III breast cancer completed, with 6 or more months having elapsed between treatment and first documented local or distant disease recurrence; TNBC status and tumor PD-L1 combined positive score confirmed centrally; and measurable disease by CT or MRI per RECIST v1.1 criteria. Additionally, patients with an ECOG performance status of 0 or 1 and adequate organ function were eligible for enrollment.
References
- Trodelvy plus Keytruda demonstrates a statistically significant and clinically meaningful improvement in progression free survival in patients with previously untreated PD-L1+ metastatic triple-negative breast cancer. News release. Gilead Sciences Inc. April 21, 2025. Accessed April 21, 2025. https://tinyurl.com/3r97auu4
- Study of sacituzumab govitecan-hziy and pembrolizumab versus treatment of physician's choice and pembrolizumab in patients with previously untreated, locally advanced inoperable or metastatic triple-negative breast cancer (ASCENT-04). ClinicalTrials.gov. Updated December 24, 2024. Accessed April 21, 2025. https://tinyurl.com/w6tf5pwe
- NCCN. Clinical Practice Guidelines in Oncology. Breast cancer, version 4.2025. Accessed April 21, 2025. https://tinyurl.com/43ykk3je