SBRT/Erlotinib Yield Big Improvements in Stage IV NSCLC
A small trial yielded “dramatic” results with high progression-free and overall survival using SBRT along with erlotinib for patients with stage IV lung cancer.
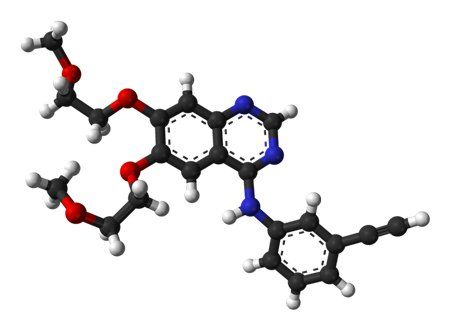
Ball-and-stick model of erlotinib.
A small trial yielded “dramatic” results with high progression-free and overall survival using stereotactic body radiation therapy (SBRT) along with erlotinib for patients with stage IV non–small-cell lung cancer (NSCLC).
“Historically, drug therapy has failed to durably control gross visible tumors in most patients,” said Robert Timmerman, MD, of the UT Southwestern Medical Center in Dallas, in an email. “In our new treatment paradigm, the SBRT, not the drugs, controls gross disease. Instead the drug is used to avoid the appearance of new tumors that would have otherwise progressed from microscopically hidden tumor.”
The new trial was a single-arm, phase II study including 24 patients with a median age of 67 years. All patients had progressed through platinum-based chemotherapy, and the median follow-up was 11.6 months. Results were published online ahead of print on October 27 in the Journal of Clinical Oncology. After erlotinib treatment began for each patient, SBRT was delivered to all disease sites.
The median progression-free survival was 14.7 months, and the median overall survival was 20.4 months. Though this trial had no comparator arm, these are substantially longer than historical studies of NSCLC patients who receive systemic therapy; typically progression-free survival and overall survival are 2 to 4 months and 6 to 9 months, respectively.
Notably, most patients eventually progressed in new distant sites, with only 3 of the 47 measurable lesions found within the SBRT fields. EGFR mutation status was evaluated in 13 of the patients, and none harbored a mutation. This suggests that, as Timmerman said, the SBRT was the driver of the longer progression-free survival rather than the drug. Including patients with EGFR mutations, the erlotinib-SBRT combination may yield even more positive results.
“The experience is exciting because the intervention seems to have dramatically changed the onset and pattern of failure,” Timmerman said. “Our 14.7 month progression-free survival means that patients had an extended ‘holiday’ from progression during which they could get on with their lives and stop having to focus on finding yet another treatment.”
He added that in some cases, patients who progressed at distant sites were kept on erlotinib and administered further SBRT; some patients have stayed on erlotinib in that way for more than 4 years.
Timmerman said that his group has proposed a larger, randomized trial using this treatment paradigm as first-line therapy in NSCLC patients. The European Organisation for Research and Treatment of Cancer (EORTC) also has plans to do a separate trial in metastatic NSCLC patients, he added. “It appears that the idea has legs.”