Screening for HPV Outperforms Pap Test for Cervical Cancer
An analysis of four randomized clinical trials from Europe shows that HPV-based screening resulted in a greater long-term protection from invasive cervical cancer compared with a Pap test.
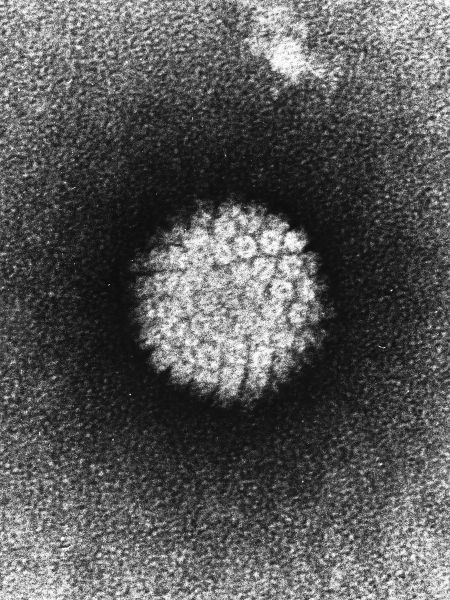
Electron micrograph of a negatively stained HPV
An analysis of four randomized clinical trials from Europe shows that human papillomavirus (HPV)-based screening resulted in a greater protection from invasive cervical cancer compared with the Papanicolaou (Pap) test, a cytology-based screening method. The results are published in the Lancet.
The detection of invasive cervical cancers was similar using both screening methods for the first 2.5 years in all four trials. But after 5.5 years of follow-up, women who's initial tests were negative had a cumulative incidence of invasive cervical carcinoma of 8.7 women per 100,000 in the HPV-screened groups, compared with 36 women per 100,000 in the groups screened by Pap smear.
Guglielmo Ronco, MD, of the Center for Cancer Epidemiology and Prevention in Turin, Italy, and colleagues pooled more than 175,000 women, aged 20 to 64, and followed them for a median of 6.5 years. The four trials used were from England (ARTISTIC), Italy (NTCC), the Netherlands (POBASCAM), and Sweden (SWEDESCREEN). A total of 107 patients had invasive cervical cancer using cancer registries and trial reports.
The authors concluded that virus-based detection results in a 60% to 70% better protection against invasive cervical cancer compared with a cytology-based test.
The results of the individual trials showed that women between the ages of 30 and 35 particularly benefited from HPV-based screening, and that HPV screening every 5 years was more protective than a Pap test every 3 years.
The rate ratios did not differ by cancer stage but were lower for adenocarcinoma (rate ratio of 0.31) compared with squamous cell carcinoma (rate ratio of 0.78). The rate ratio was lowest in the 30 to 34 year age group (rate ratio of 0.36).
“Data of large-scale randomized trials support initiation of HPV-based screening from age 30 years and extension of screening intervals to at least 5 years,” concluded the authors.
While the screening protocol differed in each trial, the effect was similar-efficacy is based on the screening test and not on the specific protocol, the authors stated.
The Pap smear procedure takes a sample of cells from the cervix which are viewed under a microscope to detect any changes that could indicate the beginning of dysplasia. Although a low-sensitivity test, the Pap test has been a very successful and relatively inexpensive cancer-screening test. In HPV-based screening, the cell sample is analyzed for the presence of HPV. The molecular techniques to detect HPV have shown to have higher diagnostic sensitivity and also reproducibility compared with cytology in detecting high-grade cervical lesion precursors, classified as cervical intraepithelial neoplasia grade 2 (CIN2) or grade 3 (CIN3).
"Until now, there have been no direct estimates of the relative efficacy of HPV-based vs cytology-based screening for prevention of invasive cancer in women who undergo regular screening, of how variables like age affect this efficacy, and of the duration of protection,” said Ronco in a statement.
In a commentary on the results, Sandra Isidean and Eduardo Franco of McGill University in Montreal, Canada, state that “the future of cervical cancer screening in high resource settings will most probably incorporate primary HPV testing.” The commentary authors also believe that with broad implementation, primary HPV screening may result in lower costs for cervical cancer screening while “providing greater safety than with conventional cervical cytology.”