Second-Line Ramucirumab/FOLFIRI Improves Survival in Metastatic CRC
Metastatic colorectal cancer patients had about a 1.5-month increase in overall survival when treated with second-line ramucirumab plus FOLFIRI vs FOLFIRI alone.
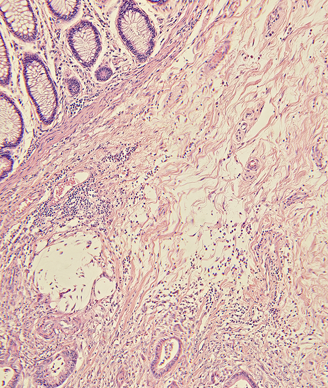
Micrograph of a colon cancer. Image © Carolina K. Smith, MD / Shutterstock.com.
Patients with metastatic colorectal cancer whose disease progressed during or after first-line bevacizumab, oxaliplatin, and fluoropyrimidine, had about a 1.5-month increase in overall survival when treated with second-line ramucirumab plus FOLFIRI compared with FOLFIRI alone, according to the results of the phase III RAISE trial.
“The benefit was consistent across subgroups, irrespective of aggressiveness of disease (progression less than 6 months vs 6 months or more after the start of first-line therapy) or tumor KRAS exon 2 mutation status,” wrote Josep Tabernero, MD, PhD, of the department of medical oncology at Vall D’Hebron University Hospital and Institute of Oncology, Barcelona, Spain, and colleagues in Lancet Oncology. “In view of our results, the combination of ramucirumab with FOLFIRI is an effective second-line treatment for patients with metastatic colorectal carcinoma.”
The RAISE trial randomly assigned 1,072 patients to 8 mg/kg intravenous ramucirumab plus FOLFIRI or placebo plus FOLFIRI every 2 weeks until disease progression, unacceptable toxicity, or death. The trial was designed to address whether continuation of VEGF inhibition, with the VEGF receptor 2 inhibitor ramucirumab, into the second-line would benefit patients treated in the first-line with the VEGF inhibitor bevacizumab.
Patients assigned to ramucirumab/FOLFIRI had a median overall survival of 13.3 months compared with 11.7 months for patients assigned placebo/FOLFIRI (hazard ratio [HR] = 0.844; 95% CI, 0.730-0.976; P = .0219). Median progression-free survival was also significantly longer in patients assigned ramucirumab/FOLFIRI compared with FOLFIRI alone (5.7 months vs 4.5 months; HR = 0.793; 95% CI, 0.697-0.903; P < .0005).
“The proportions of patients who achieved objective response were similar in the two treatment groups,” the researchers wrote. “This finding reflects those in other trials of continuation of antiangiogenic therapy after disease progression.”
The researchers noted several grade 3 or worse adverse events that occurred in patients assigned to ramucirumab/FOLFIRI and placebo/FOLFIRI, including neutropenia (38% and 23%), febrile neutropenia (3% and 2%), hypertension (11% and 3%), diarrhea (11% and 10%), and fatigue (12% and 8%).
In an editorial that accompanied the article, Timothy J. Price, MBBS, of Queen Elizabeth Hospital, Woodville, Australia, pointed out that the regimen used in the RAISE trial may not necessarily represent standard practice, as many patients do not regularly receive bevacizumab as part of their first-line treatment, and there is increased use of anti-EGFR therapies in the first line.
“The RAISE trial supports a role for targeting VEGF with ramucirumab into second-line treatment for patients who have previously received oxaliplatin, bevacizumab, and a fluoropyrimidine,” he wrote. “Whether this option will be optimum for patients previously treated with different schedules or those with RAS wild-type tumors, however, need to be addressed.”
The RAISE trial was funded by Eli Lilly.