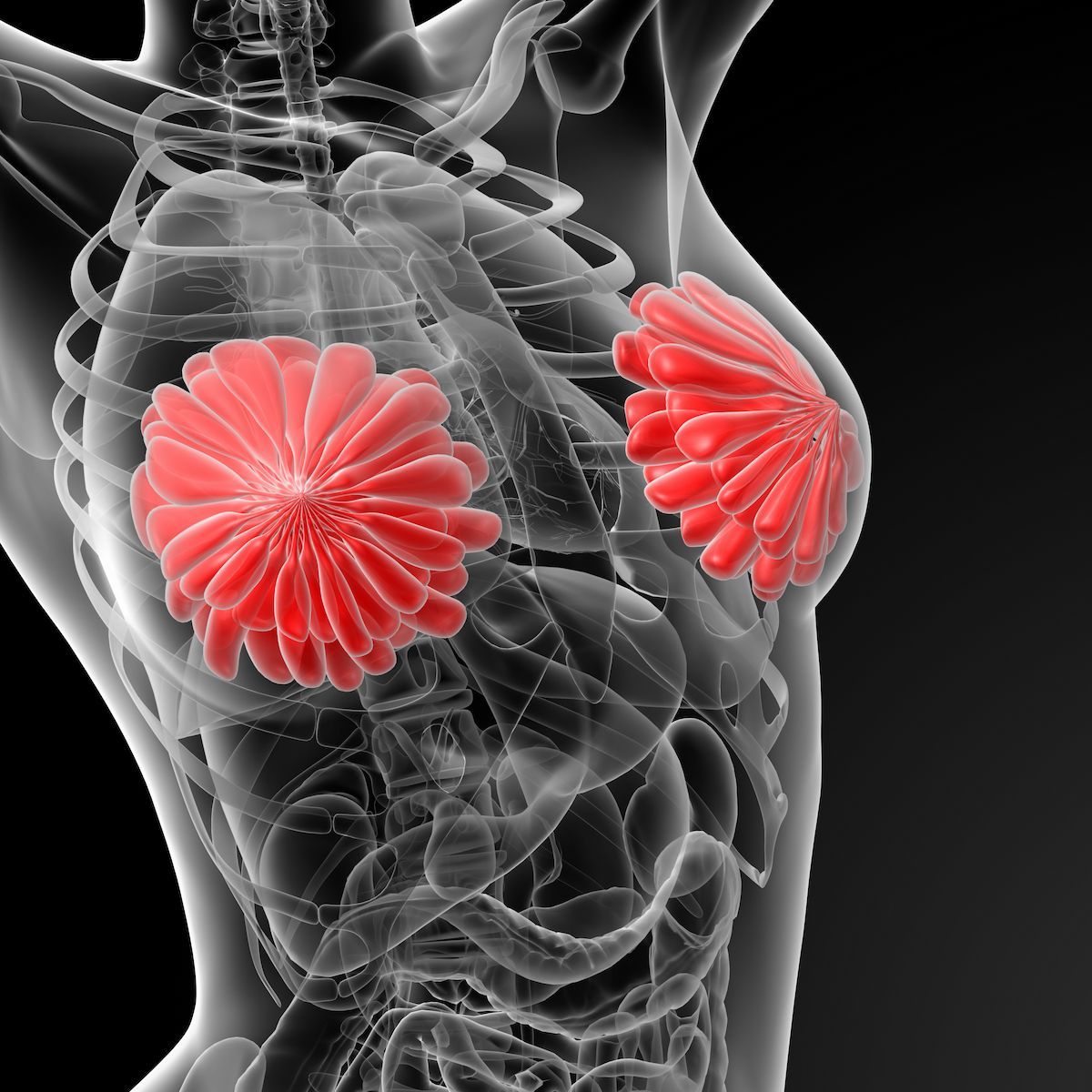
Sexual Health Considerations to Improve Survivorship in Breast Cancer
A multidisciplinary care approach should be utilized when discussing sexual health with survivors of breast cancer.
A multidisciplinary care approach should be utilized when discussing sexual health with survivors of breast cancer.
Sexual health after breast cancer is an often looked-over topic as part of a patient’s survivorship plan. Kristin E. Rojas, MD, FACS, FACOG, spoke about evidenced-based therapies to help survivors of breast cancer manage any sexual health concerns they may have.1
Rojas, assistant professor of surgery at the Dewitt Daughtry Department of Surgery, University of Miami Miller School of Medicine, and director of the Menopause, Urogenital, Sexual Health, and Intimacy Clinic (MUSIC Program) at the Sylvester Comprehensive Cancer Center, presented these findings at the 2025 Miami Breast Cancer Conference.
While the presentation focused on patients with breast cancer, Rojas noted that the MUSIC program was designed to address any concerns for women with a history of cancer. Patients are often referred to MUSIC through internal or external systems. She most commonly sees patients with breast cancer but often treats those with gynecological cancer; those who have received surgery for gastric, colon, pancreatic, peritoneal, or pseudomyxoma peritonei cancer; sarcoma; urology with Wilm’s tumor or bladder cancer; leukemia/lymphoma that is often graft-versus-host disease of the vulva/vagina; and post-stem cell transplant.
Throughout the presentation, Rojas discussed how patients were referred, the use of bioidentical hormones, vaginal rejuvenation therapy with other fringe therapies, and how this field can advance.
Diagnosis and Referral
To begin, Rojas explained that the use of anastrozole, letrozole, and exemestane block the estrogen production in fat cells. The use of chemotherapy treatments like leuprorelin and goserelin suppress the ovaries, which can trigger menopause. Additionally, the use of tamoxifen and raloxifene can interact with estrogen receptors used for breast cancer treatment.
With all these treatments, low estrogen can occur. When that does, it may lead to less lubrication or stretchiness, increased infections, vaginal pain, and spotting after sex.
The MUSIC Program has identified the most bothersome sexual function symptoms among patients seen including painful sex (35%), low libido (33%), vaginal dryness (20%), body image issues (9%), and problems with orgasm (3%).
In a presentation given by Erin Kobiella, a second-year medical student at the University of Miami for the MUSIC Program, patient characteristics and responses for other symptoms outside of vaginal dryness (55%) included painful sex (45%), low desire (36%), and hot flashes (22%). It was also noted that the ability to engage in penetrative sex was possible but uncomfortable (16%), possible but painful (66%), and impossible (18%). Changes to orgasm were either unchanged (51%), more difficult to achieve (26%), or impossible to achieve (23%).
At a presentation from the 2023 International Society for the Study of Women’s Sexual Health, Kobiella highlighted that 40% of patients experienced vaginal stenosis which included vaginal shortening (19%), adhesions/scarring (9%), and agglutination (10%).2 Other symptoms included loss of rugae (71%), vaginal pallor (76%), and vaginal dryness (84%).
“These symptoms can happen with cancer treatment at any age, are extremely common, and don’t improve with time,” Rojas emphasized.
Bioidentical Hormones
The Cleveland Clinic describes bioidentical hormones as processed hormones that are artificial to those produced by the human body and can be used to replace hormones that are low or unbalanced.3 However, there are risks to this treatment.
Rojas cited the use of long-lasting pellet therapy, called BioTe pellets made from plant-based hormone that can last up to 6 months. They are the size of a grain of rice and are inserted just under the skin. Additionally, they are marketed as something that can improve your quality of life, but she noted there has been no evidence for this.
Additional adverse effects noted in pellet therapy, likely related to supraphysiologic hormone levels, included a peak estradiol of 2 times higher than in FDA products and a peak testosterone that was 10 times higher.
The North American Menopause Society put out a statement in 2022 with their stance on hormone therapy.4 The statement noted that hormone therapy remains the most effective treatment for patients with vasomotor symptoms. However, individualized treatment should be utilized for the most benefit.
If patients are younger than 60 years old and are within 10 years of menopause onset with no contraindications, the benefit-risk ratio was favorable. If patients began treatment more than 10 years from menopause onset and were older than 60, the benefit-risk ratio was less favorable because of an increased risk of coronary heart disease, stroke, venous thromboembolism, and stroke.
Vaginal Rejuvenation
Rejuvenation options may sometimes be used in the case of vaginal prolapse or function issues. Rojas noted there should be caution around any procedures that offer surgical cures for pain or increased tightness for pleasure purposes. Rejuvenation surgery can lead to more scarring, chronic pain, bleeding, and additional surgery. Additionally, if a surgeon is not correctly trained, the removal of important body structures may occur.
The use of vaginal laser techniques is often not effective in improving sexual health functions. Most trials that highlight a perceived benefit were single-arm studies, which Rojas said can lead to a placebo effect. For those with placebo-controlled trials, there were patient-reported outcomes and histological assessments of vaginal biopsies.
In 2018, the FDA placed a warning on the use of devices that were deceptively marketed towards women for medical procedures regarding vaginal rejuvenation.5 The letter highlighted that the FDA had cleared or approved laser and energy-based devices for patients with serious conditions including the destruction of abnormal or pre-cancerous cervical or vaginal tissue in addition to condylomas. However, they were not cleared for the use of vaginal rejuvenation procedures. Most commonly, women with breast cancer who experienced early menopause were the target of this marketing.
Use of these lasers or energy-based devices for the wrong purposes was found to have caused vaginal burns, scarring, pain during intercourse, and recurring or chronic pain. At the time, the FDA had warned 7 device manufacturers of the deceptive marketing strategies, and if the concerns were not addressed, the next steps like potential enforcement actions would need to be taken.
Additionally, fringe therapies like vaginal steaming or detox pose no benefit and burns may occur. Feminine washes are also not something that should be considered for use. Jade eggs may also be recommended for pelvic floor dysfunction but should be avoided as they may worsen the patient’s condition.
Moving Forward
Looking ahead, Rojas wants her patients to have a successful sexual health journey. She outlined a few ways that can happen like eliminating irritants and assessing for vulvar dermatoses, vaginal stenosis, or fissures; using moisturizers for maintenance; utilizing lubricants for sexual activity; dilators and other devices for the pelvic floor should also be considered.
There are still questions surrounding vaginal estrogen. This is because there is no reliable evidence of increased risk of recurrence in patients with breast cancer, but a 2022 Danish study found there was a risk in a subset analysis for those on aromatase inhibitors.6
Currently, the use of vaginal estrogen is endorsed by the American College of Obstetricians and Gynecologists, the North American Menopause Society, and the American Society of Clinical Oncology.4,7,8
“When in doubt, [use] prasterone [to] non-hormonal moisturizers,” Rojas noted.
For patients who have low desire to have sex, clinicians can begin to treat vaginal dryness, pain, or pelvic floor muscle dysfunction. Treatment medications or adjustments may also be considered. Clinicians may also broach the subject of communication or relationship issues.
Overall, Rojas highlighted that sexual dysfunction is often underreported and untreated, which can lead to an environment where there are untested and unsafe therapies as treatment options. She emphasized that her colleagues should clarify any misconceptions, validate and address concerns early, begin daily moisturization, and discuss pain management.
Hormones should not be feared, but clinicians should offer multiple treatment options. The most important point is to foster multidisciplinary collaboration for better treatment of the patient.
References
- Rojas KE. Evidenced-based therapies and not-so-magic cures for sexual health concerns after breast cancer. Presented at the 2025 Miami Breast Cancer Conference; March 6-9, 2025; Miami, FL.
- Kobiella E. More than just "Vaginal Dryness": addressing an unmet need for sexual health intervention in female cancer survivors. Presented at the 2023 International Society for the Study of Women’s Health. March 5, 2023.
- Bioidentical hormones. Cleveland Clinic. Accessed March 10, 2025. https://tinyurl.com/2rwykcty
- “The 2022 Hormone Therapy Position Statement of The North American Menopause Society” Advisory Panel. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767-794. doi:10.1097/GME.0000000000002028
- Statement from FDA Commissioner Scott Gottlieb, M.D., on efforts to safeguard women’s health from deceptive health claims and significant risks related to devices marketed for use in medical procedures for “vaginal rejuvenation”. FDA. News release. July 30, 2018. Accessed March 10, 2025. https://tinyurl.com/27f6wsz6
- Cold S, Cold F, Jensen MB, Cronin-Fenton D, Christiansen P, Ejlertsen B. Systemic or Vaginal Hormone Therapy After Early Breast Cancer: A Danish Observational Cohort Study. J Natl Cancer Inst. 2022;114(10):1347-1354. doi:10.1093/jnci/djac112
- ACOG supports vaginal estrogen use for difficult symptoms in hormone-sensitive breast cancer. Living Beyond Breast Cancer. News release. September 9, 2016. Accessed March 10, 2025. https://tinyurl.com/nsb8vfbn
- Carter J, Lacchetti C, Anderson BL, et al. Interventions to address sexual problems in people with cancer: American Society of Clinical Oncology Clinical Practice Guideline Adaptation of Cancer Care Ontario Guideline. J Clin Oncol. 2017;36(5). doi:10.1200/JCO.2017.75.8995