Siltuximab New Treatment Option for Multicentric Castleman Disease
Patients with the rare and potentially deadly multicentric Castleman disease were able to achieve durable tumor and symptomatic response when assigned to treatment with the monoclonal antibody siltuximab, according to data presented at the 2013 ASH meeting.
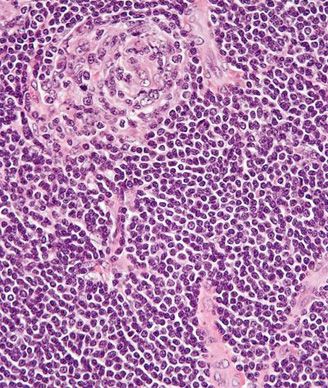
Very high magnification micrograph of Castleman disease. Copyright 2010 Nephron
Patients with the rare and potentially deadly lymphoproliferative disorder multicentric Castleman disease (MCD) were able to achieve durable tumor and symptomatic response when assigned to treatment with the monoclonal antibody siltuximab, according to data presented at the 2013 ASH Annual Meeting. One in four patients with MCD assigned to siltuximab were able to achieve complete symptom resolution.
“These results are exciting and highlight the potential for siltuximab to be a new and valuable treatment option for MCD patients who, unfortunately, had no previously available treatment options,” said Raymond S. Wong, MBChB, MD, of the Prince of Wales Hospital and the Chinese University of Hong Kong.
Research has shown that MCD signs and symptoms are driven by dysregulated interleukin-6 production. Preliminary data had suggested that siltuximab, a chimeric monoclonal antibody against human IL-6, may be effective in patients with MCD.
To explore its efficacy further, Wong and colleagues conducted a phase II multinational, double-blind, placebo-controlled study of 79 patients with MCD. Patients were randomly assigned 2:1 to best supportive care plus siltuximab (n = 53) or placebo (n = 26). Baseline symptoms of MCD disease included fatigue, malaise, night sweats, peripheral sensory neuropathy, anorexia, and pruritus. The primary endpoint was durable tumor and symptomatic response, and sustained improvement in MCD-related symptoms for 18 weeks or longer.
Patients assigned to the investigational drug had a median treatment duration of more than twice that of placebo (375 days vs 152 days). More than one-third of patients assigned siltuximab had a durable tumor and symptomatic response compared with no patients assigned to placebo (34% vs 0%; P = .0012). In addition, the median duration of tumor and symptomatic response was 340 days.
At the time of the analysis, patients assigned siltuximab had not yet reached the median time to treatment failure and the median time to next treatment. Fifty-seven percent of patients in the investigational arm achieved durable symptomatic response with 25% of them achieving complete symptom resolution for a median of 1.3 years. Only 19% of patients in the placebo arm had durable symptom response (P = .0018).
“When looking at laboratory parameters, patients on siltuximab showed rapid and significant reduction in all inflammatory markers,” Wong said.
Sixty-one percent of patients assigned siltuximab had hemoglobin improvements of 15 g/L or more at week 13 compared with no patients assigned placebo (P = .0002). Sustained decreased in C-reactive protein, erythrocyte sedimentation rate and fibrinogen were all seen among patients assigned the investigational drug.
Overall, the frequency of adverse events appeared to be similar between the placebo and siltuximab despite the duration of treatment of siltuximab being twice that of placebo, Wong said.
“If siltuximab gains regulatory approval, this experimental therapy could become the first globally approved treatment for this incurable disease and could potentially transform how patients are treated in the future,” Wong said in a press release.