Src Activity Increased in GIST
Results of a small study indicate that patients with gastrointestinal stromal tumors had increased activity of Src, but unlike in other tumors, it may be associated with longer overall survival.
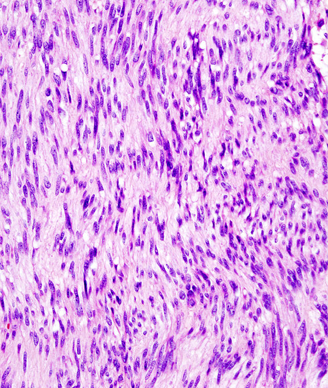
Histopathologic image of gastric GIST. Source: KGH, Wikimedia Commons
Results of a small study indicate that patients with gastrointestinal stromal tumors (GIST) had increased activity of Src, a non-receptor protein tyrosine kinase found in a variety of other solid tumors.
However, researchers led by Julia Valerie Rotert, MD, of Heidelberg University, Mannheim, Germany, pointed out that in contrast to many of the other tumors where Src activity is seen, in GIST, presence of Src was not correlated with poor clinical outcome. Instead, results of this study, published in the Journal of Surgical Oncology, indicated that Src may be associated with longer overall survival.
The majority of GIST tumors develop due to a mutation of the KIT-receptor, leading to tumor cell proliferation. Patients with GIST are traditionally treated with imatinib; however, research is being conducted into the use of multi-tyrosine kinase inhibition using Src family kinase inhibitors, particularly in patients who develop resistance to imatinib.
Rotert and colleagues sought to understand more about Src activity in patients with GIST. They analyzed tissue for 29 patients with GIST who had undergone surgery at Heidelberg University between April 2003 and January 2006. Patients were followed for a median of 11 months.
Tissue analysis showed that patients with GIST had a significant increase in Src activity (P = .093). The researchers found that Src activity was higher among those patients who had survived compared with those who died during follow-up (P = .042). Additionally, primary tumors were found to have increased Src activity compared to recurrent tumors and metastases (P = .04).
When the researchers isolated the data to only those 16 patients who had no response to imatinib therapy, Src activity was found to be significantly higher in the tumor compared with normal tissue (P = .017). According to the researchers, “this suggests that imatinib might have an influence on Src activity, or that Src might have an influence on imatinib response.”
Trends were seen for longer disease-specific survival and overall survival for patients with high Src activity, with response to imatinib treatment as the only influencing factor on overall survival.
“This supports the hypothesis that elevated Src activity might improve imatinib response, or that Src activity might be downregulated during therapy with imatinib,” the researchers wrote. “To completely understand the role of Src in GIST and the molecular mechanisms behind their clinical behavior, and to clarify what kind of functional role Src plays in GIST, further mechanistic investigations are warranted in the future.”