Staging System Revised for Multiple Myeloma
The International Myeloma Working Group has published a revised International Staging System for multiple myeloma that incorporates chromosomal abnormalities.
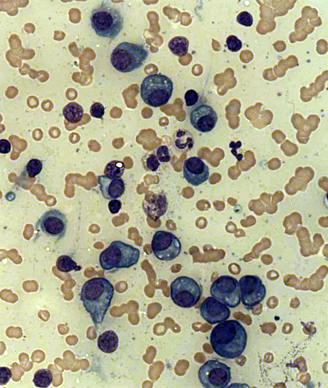
Plasma cells in a case of multiple myeloma; source: Dr. Erhabor Osaro
The International Myeloma Working Group recently published the details of a revised International Staging System (R-ISS) for multiple myeloma that incorporates the original staging system with chromosomal abnormalities (CA) detected by interphase fluorescent in situ hybridization after CD138 plasma cell purification and serum lactate dehydrogenase (LDH).
“The R-ISS staging system is a new risk stratification algorithm with an improved prognostic power compared with the individual ISS, CA, and LDH parameters,” Antonio Palumbo, MD, of Azienda Ospedaliero-Universitaria Città della Salute e della Scienza di Torino, and colleagues wrote in the Journal of Clinical Oncology. “It includes simple, reliable, and widely used prognostic markers, and it allows the identification of three different multiple myeloma entities with clearly different outcomes.”
These three new multiple myeloma entities are:
♦ R-ISS I: serum beta2-microglobulin level < 3.5 mg/L and serum albumin level of 3.5 g/dL or greater, no high-risk CA [del(17p) and/or t(4;14) and/or t(14;16)], and normal LDH level (less than the upper limit of normal range);
♦ R-ISS III: includes ISS stage III (serum beta2-microglobulin level > 5.5 mg/L) and high-risk CA or high LDH level;
♦ R-ISS II: which includes all other possible combinations.
To establish these new groups, the International Myeloma Working Group used data from 4,445 patients with newly diagnosed multiple myeloma taken from 11 international trials. Data for ISS, CA, and LDH were available for 3,060 of the patients. The researchers developed an algorithm that adjusted for all three of these factors, allowing for “a better evaluation of patient prognosis,” adding that one in four patients would have been incorrectly allocated to a good prognosis group if only one of the three factors had been considered.
With a median follow-up of 46 months, the 5-year overall survival was 82% for patients classified as R-ISS I, 62% for R-ISS II, and 40% for R-ISS III. The 5-year progression-free survival was 55%, 36%, and 24%, respectively.
A multivariable analysis for overall survival was conducted adjusting for age, sex, and R-ISS. Using this model, the risk of death was increased for age more than 65 years (hazard ratio [HR], 1.32 [95% confidence interval (CI), 1.14–1.52]; P < .001), male sex (HR, 1.16 [95% CI, 1.02–1.33]; P < .029), R-ISS stage II vs I (HR, 3.59 [95% CI, 2.68–4.80]; P < .001), and R-ISS stage III vs I (HR, 9.64 [95% CI, 6.24–4.88]; P < .001).
“There is a clear need for a better differentiation of patients with multiple myeloma. Multiple myeloma can no longer be considered a single disease, but a mix of different disease entities,” the researchers concluded. “Today, new treatments are available, and survival of patients with multiple myeloma has significantly improved. In clinical practice, a better definition of multiple myeloma subgroups is essential to provide more effective personalized therapies.”