Statin Use Improved Survival Post-Nephrectomy for RCC
The use of statins was independently associated with improvements in overall survival and disease-specific survival among a group of patients who had undergone partial or radical nephrectomy for renal cell carcinoma.
The use of statins was independently associated with improvements in overall survival and disease-specific survival among a group of patients who had undergone partial or radical nephrectomy for renal cell carcinoma (RCC), according to the results of a new study.
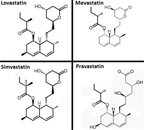
Chemical structure of statins
The study was presented by Peter E. Clark, MD, associate professor of urologic surgery at Vanderbilt-Ingram Cancer Center, during a moderated poster session at the 108th Annual Meeting of the American Urological Association, in San Diego.
“This retrospective study suggests those taking statins may have a higher survival rate following surgery for RCC,” said Scott Eggener, MD, the session’s moderator and associate professor of urologic oncology at the University of Chicago Medical Center, in a press release. “Given that one in four Americans over 45 years of age take a statin, and RCC occurs most often in men ages 50–70, it may be prudent to prospectively evaluate if statins protect against progression after RCC treatment.”
Prior research has shown a protective effect of statins in relation to other cancer types, including prostate cancer; however, no research had looked at the effect of the drugs in post-surgical renal cancer. Clark and colleagues conducted a retrospective study of statin use among 967 patients who had undergone nephrectomy between 1995 and 2010. The patients were followed for a median of 42.9 months.
Among patients who had taken statins, the median disease-specific survival rate was 90% (95% CI, 86%–93%) compared with 83% (95% CI, 80%–86%) among those who did not take statins (P = .045).
Data from the patients indicated that statins were independently associated with an improvement in overall survival (HR = 0.60; 95% CI, 0.42–0.86) and disease-specific survival (HR = 0.48; 95% CI, 0.28–0.81) compared with non-users, even after adjustments for age, American Society of Anesthesiologists physical status, T-stage, nodal status, metastases, grade, anemia, hypercalcemia, and ABO blood group.
“Further work is needed to clarify the biologic mechanism behind this association, which may depend on modulation of immune function by statins,” the researchers concluded.