Study: Fertility Drugs Not Linked to Increased Breast Cancer Risk
After a 30-year follow-up, it was shown that women treated with fertility drugs did not have an increased risk of breast cancer compared with women not exposed to the treatments.
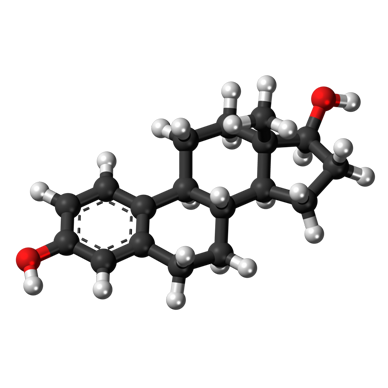
Ball-and-stick model of estradiol, which has previously been linked to increased breast cancer risk
After a 30-year follow-up, it was shown that women treated with fertility drugs did not have an increased risk of breast cancer compared with women not exposed to the treatments. The results of this National Cancer Institute–funded study were published in Cancer Epidemiology, Biomarkers & Prevention, a journal from the American Association for Cancer Research (AACR).
Previous epidemiological studies have shown conflicting results on the link between breast cancer risk and use of fertility drug treatments, from increased and decreased risk, to no association. Some of these previous studies have also not been able to account for risk factors for breast cancer, such as family history and reproductive status. Previous studies have linked fertility treatments to increased ovarian cancer risk.
The study followed a cohort of 12,193 women who were evaluated or treated for infertility between 1965 and 1988. Through 2010, data were available for 9,892 (81.1%) patients in the cohort. Women were treated with either clomiphene citrate or gonadotropins.
During the median 30 years of follow-up, 749 breast cancer cases were observed. The average age of the participants at time of breast cancer diagnosis was 52.7 years. In the 38.1% of patients who received clomiphene citrate treatment, risk of breast cancer was found to be no more likely than in those who had never been treated with the drug (hazard ratio [HR] = 1.05).
“Overall, our data show that use of fertility drugs does not increase breast cancer risk in this population,” said lead author Louise A. Brinton, PhD, MPH, chief of the hormonal and reproductive epidemiology branch at the National Cancer Institute in Bethesda, Maryland.
These results are similar to those from the authors’ previous report after a median 18.8-year follow-up.
There was a slight increased risk among women who received 12 or more cycles of clomiphene citrate (HR = 1.37). There was also a slight increase in risk observed among those women who first received clomiphene citrate at age 35 or older (HR = 1.31).
Current practice is to expose women to a maximum of 3 to 6 cycles of clomiphene citrate at doses up to 100 mg, which is lower than past clinical practice.
“We did note that among women who were unable to become pregnant, there were higher risks for those who had taken gonadotropins or clomiphene citrate as compared with those who never took either medication,” said Brinton.
Patients who had multiple cycles of clomiphene citrate had a higher risk of breast cancer, even after taking additional breast cancer risk factors into account (HR = 1.69).
Among 9.6% of the women who were treated with gonadotropins, a significant relationship of gonadotropin use and invasive cancer was seen among the women who had never been pregnant (HR = 1.98). Gonadotropin use was mainly in combination with clomiphene citrate. The study did not evaluate the use of gonadotropins for in vitro fertilization, which is currently used in the clinic.
Still, this observed increased breast cancer risk in women who received multiple fertility treatment cycles and were unable to become pregnant may be related to persistent infertility rather than an effect of the fertility medications, noted Brinton.
“These findings stress the importance of continued monitoring of women who are exposed to fertility drugs,” said Brinton.
One of the proposed mechanisms of the link between breast cancer and fertility drugs is the increase in estradiol levels, which have previously been linked to increased breast cancer risk. But, more research is necessary to understand the potential biological mechanisms of how fertility drugs could influence breast tumor formation.
Brinton and colleagues are continuing to monitor the women in this long-term study to evaluate the increased risk observed among subsets of women in the study, particularly since the cohort is relatively young and have not reached their peak incidence for breast cancer.