Study Links Later-Generation BRCA Mutation Carriers with Earlier Breast and Ovarian Cancer Onset
The results of a study that tracked BRCA mutation carriers suggest that women who inherit BRCA gene mutations develop cancer at a younger age than women in the previous generation. The study is published on-line today in the journal Cancer.
The results of a study that tracked BRCA mutation carriers suggest that women who inherit BRCA gene mutations develop cancer at a younger age than women in the previous generation. The study is published online today in Cancer, a journal of the American Cancer Society (DOI:10.1002/cncr.26284).
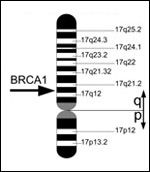
BRCA1
gene, located on chromosome 17, Courtesy of Armin Kbelbeck, Wikimedia Commons
The authors analyzed 132 BRCA-positive “generation 2” women with breast cancer who were treated at the University of Texas M.D. Anderson Cancer and their 106 “generation 1” family member who had also been diagnosed with BRCA-related breast or ovarian cancer. The goal of the research was to assess whether later-generation BRCA-mutation carriers are more likely to have earlier-onset of these cancers; one of the major risks for hereditary breast and ovarian cancer syndrome (HBOC) for BRCA-mutations carriers is the development of breast cancer at a young age. All families evaluated had been referred to the Clinical Cancer Genetic Program at M.D. Anderson and previous generation non-HBOC cancers were not included in the study cohort.
Autosomal-dominant inherited BRCA1 and 2 mutations are responsible for approximately 5% to 10% of breast cancer diagnoses. Carriers of BRCA mutations have an elevated risk of both breast and ovarian cancer development, with a life-time risk of 47% to 66% and 40% to 57% for breast cancer in BRCA1 and BRCA2 carriers, respectively. The risk for ovarian cancer is estimated to be between 35% to 46% and 13% to 23% for BRCA1 and BRCA2 carriers, respectively. Therefore, better data on the age of cancer onset and patterns of inheritance will facilitate our understanding of the role of these genes in cancer.
Among the 303 women in at least 2 generations that were analyzed, the median age of cancer diagnosis was 42 years in generation 2 and 48 years of age in generation 1 (P < .001). The statistical analysis accounted for the differences in medical care by decade of birth spanned by the women in the study cohort. Using a different statistical model, the authors found that the change in the expected age of cancer onset decreased by 7.9 years from the first to the second generation. “This study shows that this will be an important factor to closely follow forward” in HBOC, says Jennifer K. Litton, MD of the department of breast medical oncology at M.D. Anderson, one of the lead authors of the study.
“Our research tells us that we need to continue to initiate screenings at least ten years prior to the earliest cancer diagnosis,” said Dr. Litton “Also, because we do not have the BRCA mutation status of affected individuals from previous generations, when testing may not have been available yet, it is vital that we continue to collect family information,” she added. Continuing to accumulate the data in shifts in age of diagnosis will allow for more accurate timing of guidance and intervention in future generations. Currently the NCCN guidelines recommend screening starting at ages 20 to 25, or five to ten years earlier than the youngest age at diagnosis of a family member. The authors believe that based on their work and previous evidence, the current guidelines are sufficient.
The authors note that although each generation subset was small in this study, the result is further evidence of genetic anticipation in HBOC. Anticipation is the earlier onset and increased severity of certain genetic disease in subsequent generations and has been observed in fragile X syndrome and Huntington’s disease. Anticipation has been suggested in breast cancer, but so far, study cohorts have been small. The idea that anticipation may occur in HBOC is logical as the BRCA proteins function in genomic stability and DNA repair pathways and so far, the evidence in fragile X and Huntington’s disease points to DNA instability as being responsible for the anticipation phenomenon.
This study has several limitations and subsequent data collection from more patients in future generations will facilitate the clarification of the authors’ conclusions. The study did not analyze the role of environmental factors such as various exposures, geography, patient race, and lifestyle choices. It would be interesting but complicated to see how environmental factors play a role in HBOC. According to Litton, “We could not really control for geography. We included women who were seen in our genetics clinic and either had a personal or familial history of cancer.”
Additionally, the data may be biased by the disparity in screening timing and better techniques, as younger generations are much more aware of breast and ovarian cancers, are likely more pro-active about screening processes, and have had screenings with much better imaging tools.
The fact that the analysis only considered patients at as single institution may have created bias as well. The authors do highlight this point, stating that M.D. Anderson is a tertiary cancer center with a younger patient base compared to the general population with breast cancer.
Regardless of these caveats, however, this study and subsequent ones will facilitate our understanding of the role of BRCA in hereditary ovarian and breast cancers to allow for better screening and subsequent treatment. In parallel to this type of analysis, Dr. Litton says that she and her colleagues are also "working on many translational projects to look at underlying causes for cancer in people with a BRCA mutation.” The clinical cancer genetics clinic at M.D. Anderson is also actively doing similar research in other cancers that have a known link with a genetic cause.