Study Validates Prognostic Value of mTOR Pathway Markers in RCC
An external validation study has confirmed that biomarkers of the mTOR pathway have prognostic value in patients with clear cell renal cell carcinoma.
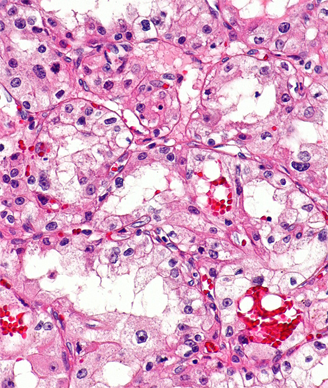
Micrograph of clear cell RCC; source: Nephron, Wikimedia Commons
An external validation study has confirmed that biomarkers of the mammalian target of rapamycin (mTOR) pathway have prognostic value in patients with clear cell renal cell carcinoma (RCC) and may help physicians to identify those patients who could benefit from additional treatments.
“Molecular markers have the ability to discriminate between tumors of varying biologic potential and can aid in clinical risk stratification,” Ahmed Q. Haddad, MD, PhD, of the University of Texas Southwestern Medical Center, and colleagues wrote in Cancer. “Molecular staging also has the advantage that it can be performed preoperatively on tissue biopsy specimens and may therefore have benefit in augmenting treatment decisions.”
In prior research, researchers from the University of Texas Southwestern Medical Center reported on a panel of mTOR markers that were associated with aggressive tumor biology and inferior outcomes. The panel included phosphorylated-S6, phosphorylated-mTOR (p-mTOR), mTOR, phosphorylated-AKT, hypoxia inducible factor-1α, Raptor, phosphatase and tensin homolog (PTEN), phosphoinositide 3-kinase (PI3K), and phosphorylated 4E-binding protein-1 (p-4EBP1).
In this study, Haddad and colleagues sought to further validate the value of these markers. They performed immunohistochemistry for five markers-PTEN, PI3K, p-mTOR, phosphorylated-S6 (p-S6), and p-4EBP1-on tissue microarrays from 528 patients with non-metastatic clear cell RCC treated surgically at four centers. The patients had a median follow-up of 56.5 months.
At follow-up, 14.4% of patients had disease recurrence, 9.7% of patients had died of the disease, and 7.4% died from other causes. All patients examined had alteration of at least one of the markers. Specifically, 52.7% had alteration of PI3K; 77.5%, PTEN; 25.4%, p-mTOR; 86.4%, p-4EBP1; and, 29.7%, p-S6.
Results of a multivariate analysis that adjusted for stage, grade, and nodal status showed that alterations in p-4EBP1 and p-S6 were associated with worse recurrence-free survival (hazard ratio [HR] = 2.81; 95% CI, 1.21-6.53; P = .02; and HR = 1.92; 95% CI, 1.19-3.11; P = .01, respectively).
The researchers also noted a strong association with recurrence-free survival and the total number of altered biomarkers. Patients with 4–5 altered biomarkers had a significantly increased HR for recurrence-free survival compared with those patients with 0–1 altered biomarkers (HR = 3.20; P = .02 for patients with a high vs low 5-biomarker score).
The researchers also evaluated the benefit of looking at only those two alterations that showed significant association with recurrence-free survival on univariate analysis (p-S6 and p-4EBP1). The panel consisting of these two markers independently predicted for worse recurrence-free survival (HR = 4.38; P = .003 for patients with a high vs low 2-biomarker score).
“The 2-marker score improved the AUC from 0.772 to 0.782, and the net reclassification improvement was significant (0.357, P = .004), demonstrating that the addition of the 2-marker score significantly improved the classification of predicted risk of recurrence compared with the baseline clinical model incorporating stage, grade, and lymph node status,” the researchers wrote. “These findings suggest that future validation studies could utilize the abbreviated 2-marker scoring system, which would be more cost effective and easier to implement than the 5-marker panel.”