Surgery Trends Towards Improved Outcomes Vs SABR in Elderly NSCLC Group
Factors such as World Health Organization status appeared to correlate with early mortality in an elderly non–small cell lung cancer cohort.
“[O]ur results seem to confirm a trend towards superiority of surgery in terms of [OS] and locoregional control, with nonetheless excellent disease control and tolerability after SABR," according to the study authors.
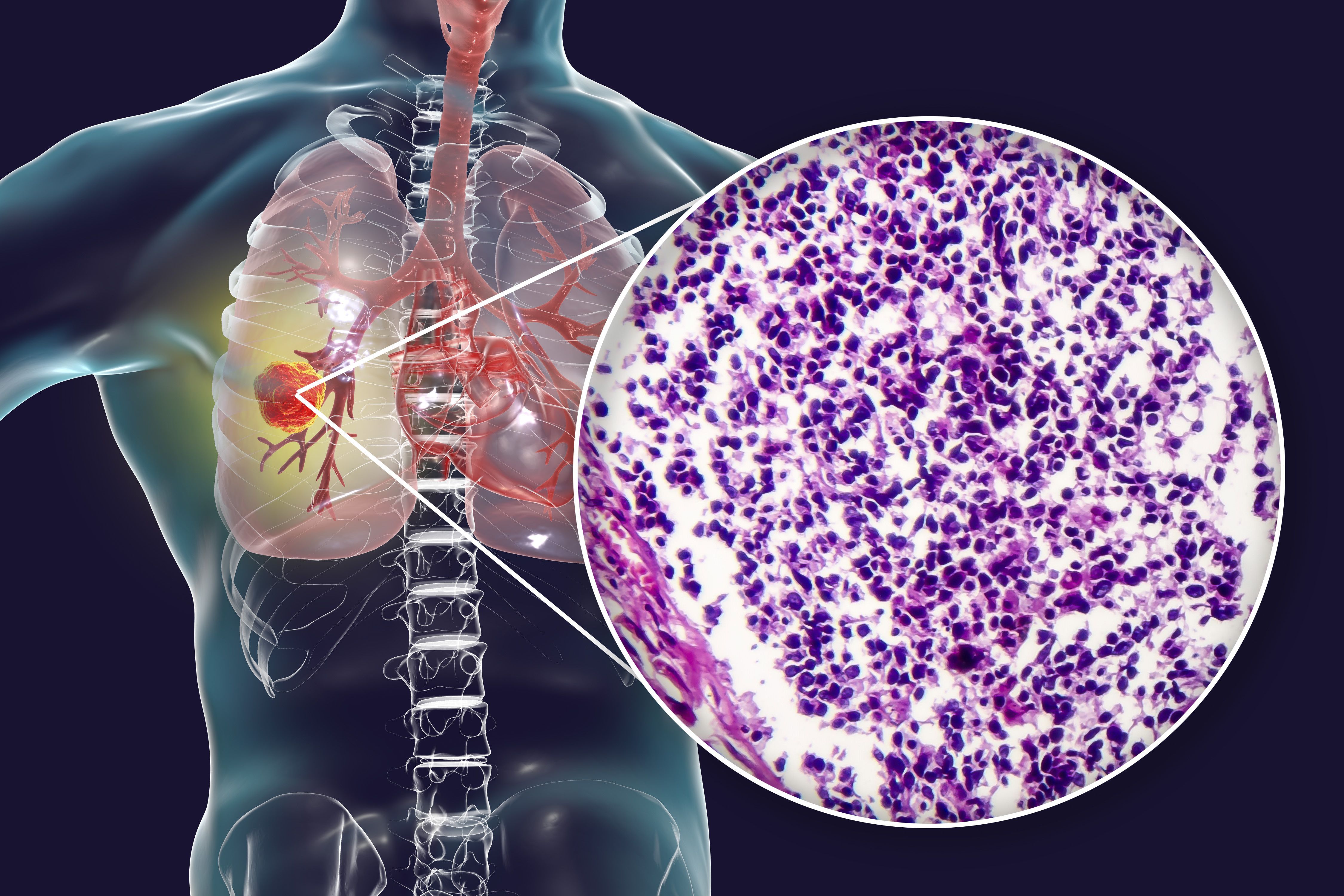
Surgery trended towards improved overall survival (OS) and locoregional control vs stereotactic radiotherapy (SABR) among elderly patients with non–small cell lung cancer (NSCLC), according to findings from a retrospective study published in Cancers.1
Before matching in the global population, the OS rates with surgery and SABR, respectively, were 89.6% (95% CI, 86.1%-93.4%) and 89.59% (95% CI, 83.7%-95.9%) at 1 year, 77.06% (95% CI, 71.6%-82.9%) and 52.95% (95% CI, 42.7%-65.6%) at 3 years, and 61.28% (95% CI, 54.0%-69.5%) and 27.32% (95% CI, 17.1%-43.7%) at 5 years (P <.0001). Following matching, the 1-year OS rates were 83.87% (95% CI, 77.4%-90.8%) and 88.8% (95% CI, 82.2%-96.0%), the 3-year rates were 73.61% (95% CI, 65.2%-83.1%) and 57.1% (95% CI, 46.3%-70.4%), and the 5-year rates were 47.30% (95% CI, 36.1%-62.0%) and 31.5% (95% CI, 19.9%-49.9%) in each respective group (P = .068).
Multivariate analysis indicated that World Health Organization (WHO) status significantly impacted OS outcomes (HR, 2.53; 95% CI, 1.38-4.70; P = .003). Treatment strategy did not significantly correlate with OS.
The rate of locoregional recurrence in the general population was 9.4% (n = 27; 95% CI, 6.4%-13.5%) among patients who received surgery vs 22.8% (n = 23; 95% CI, 15.2%-32.4%) among those who were treated with SABR (P = .001). Following matching, these rates were 11.8% (n = 15; 95% CI, 7.9%-21.4%) and 21.2% (n = 18; 95% CI, 13.3%-31.6%) in each arm.
The likelihood of survival without locoregional recurrence (EFLRS) in the surgery and SABR groups, respectively, was 93.1% (95% CI, 88.4%-98.2%) compared with 94.5% (95% CI, 89.4%-99.9%) at 1 year and 89.4% (95% CI, 83.3%-95.9%) vs 64.7% (95% CI, 52.1%-80.3%) at 3 years (P = .052). When considering death as a competing risk in the occurrence of local recurrence, investigators noted a smaller contrast in outcomes between the 2 arms (HR, 1.73; 95% CI, 0.878-3.41; P = .11).
“[O]ur results seem to confirm a trend towards superiority of surgery in terms of [OS] and locoregional control, with nonetheless excellent disease control and tolerability after SABR. Our study highlights the strong impact of early death after surgery,” Galdric Oliver, of the Oncology Radiotherapy Department, CRCM Inserm, Genome Instability and Carcinogenesis, Assistance Publique des Hôpitaux de Marseille, Aix Marseille University, wrote with study coauthors.1 “We believe that the future challenge for this population lies in a more relevant therapeutic selection. In this context, we are proposing for the first time a therapeutic decision support tool to improve the selection of patients eligible for surgery and thus further improve the [OS] of this population.”
According to the study authors, lobectomy plus lymph node dissection represents a standard choice for patients with stage IA to IIA NSCLC. However, they noted SABR as an option for those who are not eligible for surgical resection and as an alternative to surgery for patients with operable disease in whom other causes of mortality associated with comorbidities compete with those related to cancer.2
Investigators of this single-center retrospective study compared surgery with SABR in the treatment of patients 75 years and older who received routine care for stage IA to IIA NSCLC. Propensity matching was employed to ensure that the surgery and radiotherapy groups were comparable by matching parameters including tumor size, sex, age, comorbidity index, and WHO status.
Patients who underwent surgery received a thoracotomy, a multiport video-assisted thoracoscopy, or a 3- or 4-arm robot-assisted thoracoscopy. Radiotherapy initially consisted of TomoTherapy® at 60 Gy in 5 fractions from 2012 to 2019. Following protocol modifications, patients in the radiotherapy population received treatment with the Cyberknife® from 2020 to 2022.
The study’s primary end point was OS. Other disease-specific outcomes of interest included EFLRS and metastatic progression. Additionally, investigators performed a CART decision tree analysis to identify groups of patients who may be at risk for OS and early death.
Before matching, the study population included 288 elderly patients who underwent surgery and 101 who received SABR at Marseille University Hospital from January 2012 to December 2022. Performance status, comorbidity index, and respiratory function criteria appeared to favor patients in the surgery group prior to matching.
The matched population included 127 patients in the surgery group and 85 in the radiotherapy group. Most patients in each respective group were male (70.1% vs 67.1%; P = .753) and had a WHO status of 1 (45.7% vs 45.9%; P = .081). The most common tumor stage was IA (84.3% vs 84.7%).
Metastatic recurrence was reported in 7.6% (n = 22) of the surgery group and 5.9% (n = 6) of the SABR group across the general population. Following matching, the rates of metastatic recurrence were 8.6% (n = 11) and 5.8% (n = 5) in each respective treatment group.
Deaths within 90 days of treatment occurred in 8.3% (n = 10; 95% CI, 4.0%-14.4%) of the surgery group and 1.2% (n = 1; 95% CI, 0.06%-7.3%) in the SABR group across the general population (P = .063). Additionally, 8.7% of patients who underwent surgery required readmissions for complications related to treatment.
A CART subgroup analysis indicated that carbon monoxide diffusion capacity (DLCO) and comorbidity index had a major impact on OS. Investigators identified 3 distinct subgroups based on respiratory function, WHO status, and comorbidities within the matched population.
“After subgroup analysis using the CART method, we are proposing a therapeutic decision aid for elderly patients already considered eligible for surgery. This decision aid, which considers gender, WHO status, and forced expiratory volume in 1 second [FEV1] status, will make it possible to redirect these patients eligible for surgery towards SABR and thus help to improve their [OS],” the authors wrote.1
References
- Oliver G, Boucekine M, Couderc A-L, et al. Surgery versus stereotactic radiotherapy in patients over 75 years treated for stage IA–IIA NSCLC. Cancers. 2025;17(4):677. doi:10.3390/cancers17040677
- Vansteenkiste J, Crinò L, Dooms C, et al. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann Oncol. 2014;25(8):1462-74. doi:10.1093/annonc/mdu089