TAR-200 Yields Complete Responses in BCG-Unresponsive High-Risk NMIBC
Efficacy and safety data from the phase 2b SUNRISE-1 trial support the ongoing evaluations of TAR-200 as a treatment for patients with BCG-unresponsive high-risk non–muscle-invasive bladder cancer.
"The efficacy and safety data from SUNRISE-1 [NCT04640623] support the ongoing investigations of TAR-200 in patients with BCG-unresponsive, high-risk NMIBC," according to Andrea Necchi, MD.
Investigators reported sustained complete responses (CRs) in patients with BCG-unresponsive, high-risk non–muscle-invasive bladder cancer (NMIBC) treated with TAR-200, according to findings from the phase 2b SUNRISE-1 trial (NCT04640623) presented at the 2023 European Society for Medical Oncology Congress (ESMO).1
TAR-200 achieved a CR rate per central review of 76.7% (95% CI,57.7-90.1), consisting of 23 CRs in 30 evaluable patients. The investigator-assessed CR rate was similar at 80.0% (95% CI, 61.4-92.3; 24 of 30 patients).
At a median follow-up of 48 weeks (range, 12-121), 21 (91%) of the 23 CRs remained ongoing and the median duration of response (DOR) was not reached. Eleven of the complete responders had a DOR of at least 6 months (10 of 11 ongoing) and 6 had a DOR of at 12 least months (all ongoing). At the time of analysis, none of the complete responders had received radical cystectomy.
“TAR-200 provides sustained and durable response. The efficacy and safety data from SUNRISE-1 support the ongoing investigations of TAR-200 in patients with BCG-unresponsive, high-risk NMIBC,” said first author Andrea Necchi, MD, associate professor at Vita-Salute Raffaele University and the head of genitourinary medical oncology at IRCCS San Raffaele Hospital and Scientific Institute in Milan, Italy.
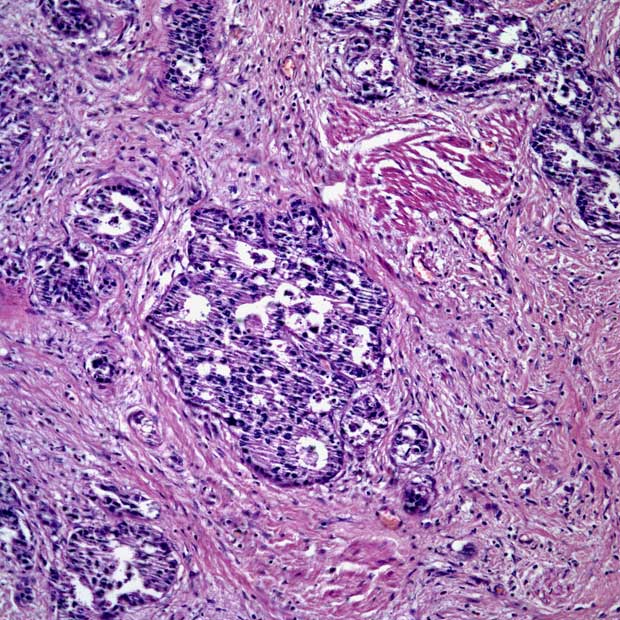
The TAR-200 intravesical delivery system works by providing sustained low-doses of localized gemcitabine via insertion into the bladder.2 The ongoing, open-label SUNRISE-1 trial is exploring the system in patients with BCG-unresponsive, histologically confirmed high-risk NMIBC (CIS with or without papillary disease) who decline to receive or are ineligible for radical cystectomy.
The initial trial design randomized patients to 3 treatment arms: cohort 1 is TAR-200 dosed every 3 weeks for up to 24 weeks, then every 12 weeks until week 96 (year 2) plus cetrelimab dosed every 3 weeks through week 78; cohort 2 is TAR-200 alone at the same dose as cohort 1; and cohort 3 is cetrelimab alone dosed at the same dose as cohort 1. The most recent amendment to the study design added a fourth cohort administering TAR-200 monotherapy to patients with BCG-unresponsive, high-risk NMIBC with papillary tumors only (no CIS component).1
CRs were measured by cystoscopy, central cytology, and central pathology at week 24 and week 48. The primary end point is CR, with secondary end points including DOR, overall survival, quality of life, safety, and tolerability.
At the ESMO Congress, Necchi only shared data from the TAR-200 monotherapy cohort (cohort 2). There were 54 patients in the cohort with a median age of 71 years (range, 40-85). The majority were male (77.8%), White (68.5%), and had an ECOG performance status of 0 (96.3%). Nicotine use data showed that 55.6% were former users, 35.2% were never users, and 9.3% were current users.
The tumor stage was CIS only for 66.7% of patients and CIS + papillary disease for 33.3% of patients. The median number of prior doses of BCG was 12 (range, 7-42). The median time from last BCG treatment to CIS diagnosis was 3.0 months (range, 0.2-22.4). The majority of patients (94.4%) declined to receive radical cystectomy and the remaining patients (5.6%) were not eligible for the surgery.
The safety population included all 54 patients. Most adverse events (AEs) were grade ≤2. Over half (53.7%) of patients had at least 1 treatment-related AE (TRAE) and 7.4% of patients had at least 1 grade ≥3 TRAE. One patient had a serious TRAE. Discontinuations due to TRAEs occurred in 2 patients. There were no patient deaths on the trial.
Beyond SUNRISE-1, TAR-200 is being investigated in several other ongoing clinical trials including SUNRISE-2 (NCT04658862) in patients with muscle-invasive bladder cancer (MIBC) who are radical cystectomy–ineligible or refuse to receive the surgery; SUNRISE-3 (NCT05714202) in patients with BCG-naive high-risk NMIBC; and SUNRISE-4 in the neoadjuvant MIBC setting (NCT04919512).
References
- Necchi A, Jacob JM, Results from SunRISe-1 in patients (Pts) with bacillus Calmette–Guérin (BCG)-unresponsive high-risk non–muscle-invasive bladder cancer (HR NMIBC) receiving TAR-200 monotherapy. Presented at: ESMO Congress 2023; October 20-24, 2023; Madrid, Spain. Abstract LBA105.
- Janssen. TAR-200 Intravesical Delivery System Results Show 77 Percent Complete Response Rate in Patients with Bacillus-Calmette-Guérin Unresponsive, High-Risk Non-Muscle-Invasive Bladder Cancer. Published online October 22, 2023. https://www.janssen.com/tar-200-intravesical-delivery-system-results-show-77-percent-complete-response-rate-patients