Tarlatamab Requires Strategic Toxicity Monitoring and Management in ES-SCLC
A real-world, retrospective analysis showed that CRS and ICANS occurred in 48% and 16% of patients with ES-SCLC who were treated with tarlatamab.
A real-world, retrospective analysis showed that CRS and ICANS occurred in 48% and 16% of patients with ES-SCLC who were treated with tarlatamab.
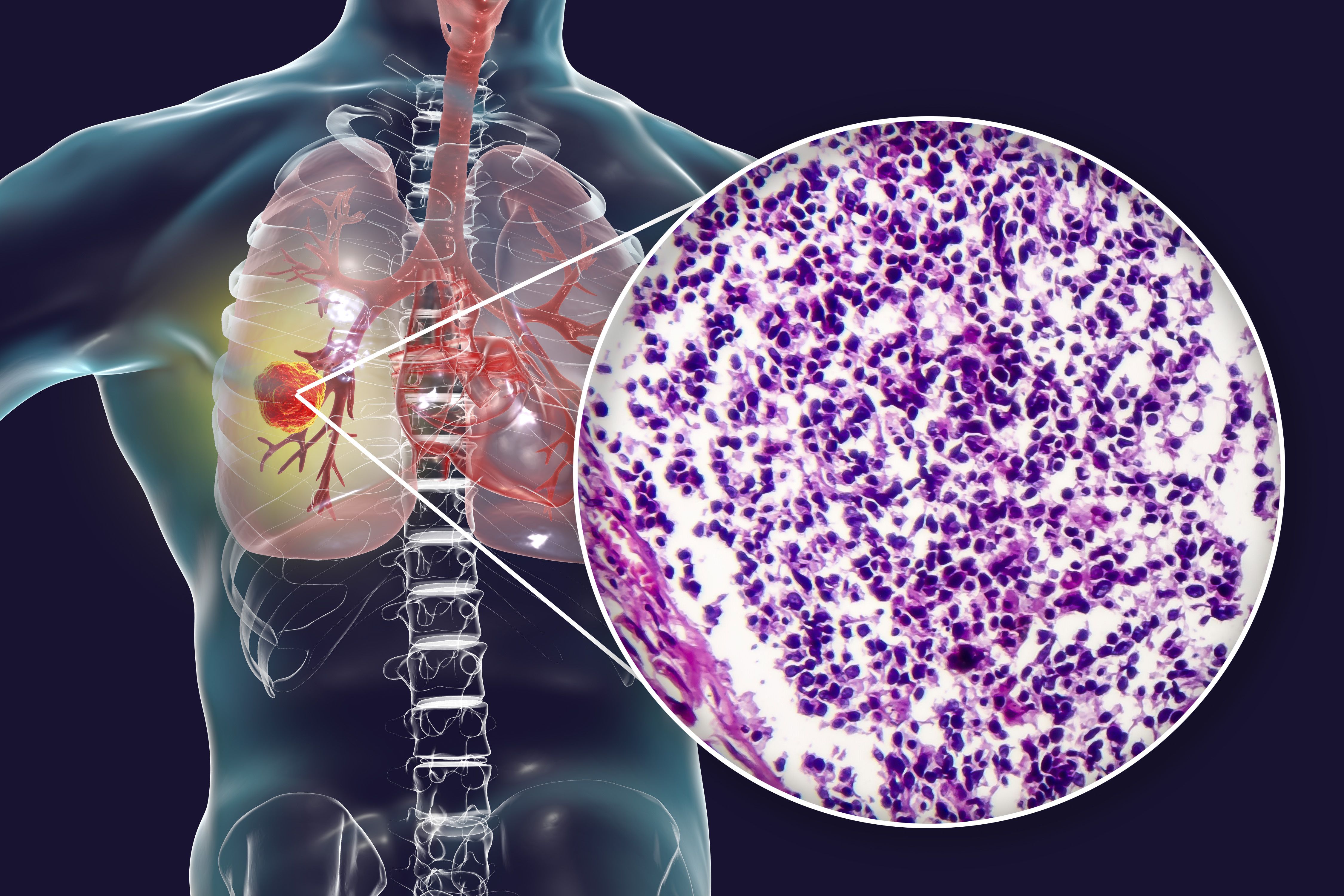
A multi-institutional real-world analysis of a small cohort of patients with extensive-stage small cell lung cancer (SCLC) found that those receiving tarlatamab-dlle (Imdelltra) as treatment should be selected carefully and monitored vigilantly, with optimized preemptive management strategies in place for treatment-related toxicities.1 These results were shared at the IASLC 2025 World Conference on Lung Cancer.
Of the 25 patients included in the retrospective cohort study, 12 patients (48%) experienced cytokine release syndrome (CRS), with all instances being grade 1/2. Immune-effector cell-associated neurotoxicity syndrome (ICANS) was observed in 4 patients (16%), with 3 instances being grade 1/2, and 1 instance being grade 3; the patient with grade 3 ICANS was admitted into the intensive care unit (ICU).
CRS onset typically occurred within 12 hours after tarlatamab infusion and was resolved with antipyretics for fever and intravenous fluids; 75% of patients who experienced CRS received corticosteroids, and no patients received an IL-6 monoclonal inhibitor therapy.
Notably, 5 patients (25%) required readmissions due to treatment-related toxicities, with a median length of stay of 2.2 days; CRS was the most common reason for hospitalization, occurring in 3 patients (60%).
Treatment was discontinued by 8 patients (32%), and 3 patients died due to disease progression within 2 cycles of treatment. Furthermore, 62% of patients discontinued therapy due to toxicity, and 15% discontinued due to progression.
“In our cohort, CRS and ICANS were predominantly low grade and mostly manageable with standard interventions. Readmissions due to treatment-related toxicities were not uncommon. There were 3 early deaths due to disease progression within 2 cycles of treatment,” wrote lead study author Estelamari Rodriguez, MD, MPH, associate director of Community Outreach – Thoracic Oncology at the University of Miami Sylvester Comprehensive Cancer Center, with coauthors, in the presentation.1 “These findings emphasize the need for patient selection, vigilant monitoring, early intervention, and potential optimization of preemptive treatment strategies.”
The trial included patients between the ages of 50 and 84 years who received tarlatamab therapy for relapsed/refractory SCLC between October 2024 and March 2025 at 2 academic centers in South Florida.
The median age of patients was 68.2 years (range, 50.0-84.0); 52% were women, and 56% were non-Hispanic. Notably, this was the largest case series of Hispanic patients with tarlatamab (44%; n = 11). Tarlatamab was received in the second line of therapy for 52% of patients, and 7 patients received at least 2 lines of therapy before tarlatamab initiation.
The primary end points of the trial were the incidence and severity of CRS, ICANS, early mortality rates, and rehospitalization events attributable to treatment-related toxicities.
The criteria used for assessing toxicity profiles were the Common Terminology Criteria for Adverse Events version 5.0; the severity of CRS was assessed via the American Society of Transplantation and Cellular Therapy consensus grading.
Currently, tarlatamab is approved by the FDA as a therapy for extensive-stage SCLC with progression on or after platinum-based chemotherapy based on the results of the phase 2 DeLLphi-301 trial (NCT05060016).2
In DeLLphi-301, the most common treatment-emergent adverse effect was CRS; it occurred in 51.1% of patients who received 10 mg of tarlatamab and 60.9% of those who received 100 mg of tarlatamab. Most CRS events were grade 1/2, with grade 3 events occurring in 1% of the 10 mg group and 6% of the 100 mg group. ICANS and associated neurological events occurred in 8% of the 10 mg group and 28% of the 100 mg group. Similarly, the majority of ICANS and associated neurological events were grade 1/2, with grade 3 events occurring in none of the 10 mg group and 5% of the 100 mg group.
“Future studies should refine toxicity mitigation protocols to enhance the safety and tolerability of tarlatamab in broader patient populations,” concluded the presentation authors.1
References
- Zuniga NM, Morgenstern-Kaplan D, Jayram DK, et al. Multi-institutional real-world experience of early tarlatamab-related toxicities for extensive stage small cell lung cancer. Presented at the 2025 International Association for the Study of Lung Cancer World Conference on Lung Cancer 2025; September 6-9, 2025; Barcelona, Spain.
- FDA grants accelerated approval to tarlatamab-dlle for extensive stage small cell lung cancer. FDA. May 16, 2024. Accessed September 18, 2025. https://tinyurl.com/48k34rw5
- Ahn MJ, Cho BC, Felip E, et al. Tarlatamab for patients with previously treated small-cell lung cancer. N Engl J Med. 2023;389:2063-2075. doi:10.1056/NEJMoa2307980