Telomere-Targeting Agent Demonstrates Tolerability in Advanced NSCLC
As of data cutoff, 6 patients with NSCLC in the phase 2 THIO-101 trial are receiving ongoing treatment with THIO plus cemiplimab after 12 months.
As of data cutoff, 6 patients with NSCLC in the phase 2 THIO-101 trial are receiving ongoing treatment with THIO plus cemiplimab after 12 months.
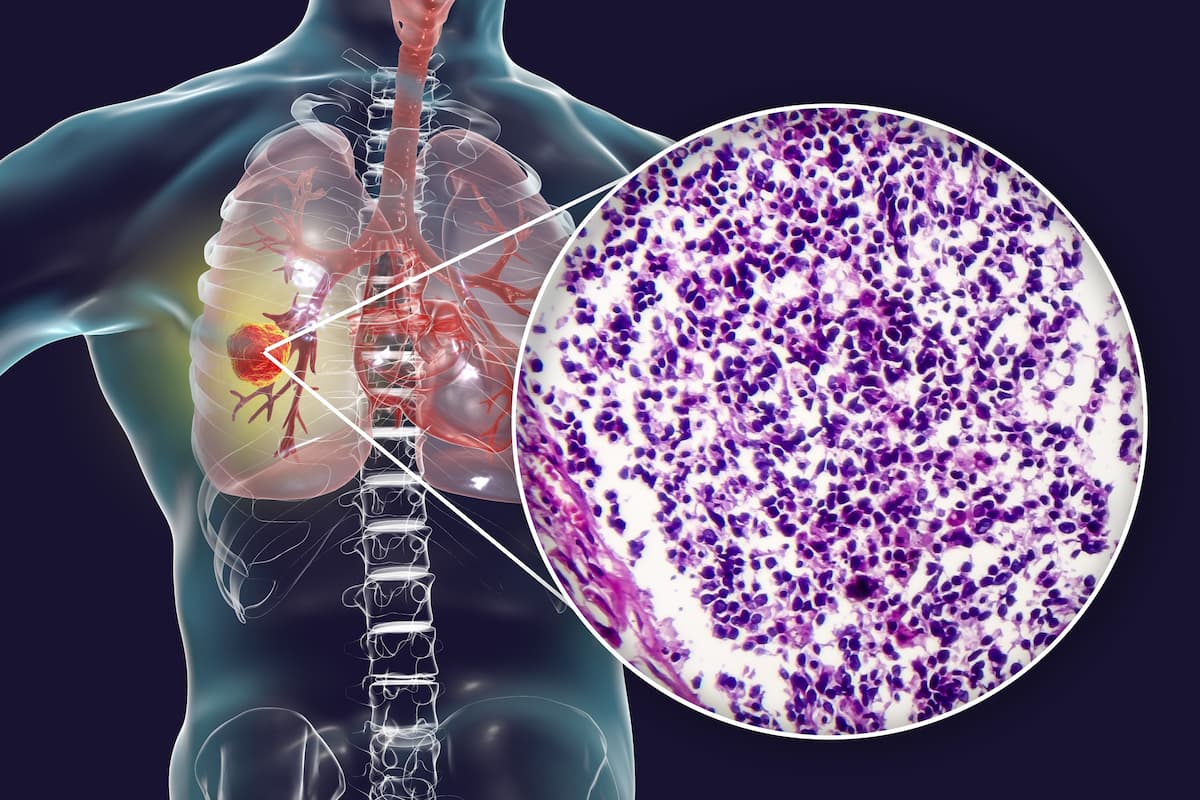
Investigational telomere-targeting agent, THIO, sequenced with cemiplimab (Libtayo) demonstrated tolerability and efficacy in patients with advanced non–small cell lung cancer (NSCLC) who progressed following 2 or more standard-of-care regimens, according to a news release from the drug’s developer, MAIA Biotechnology.1
Topline data show that after 12 months of therapy, 6 patients in the phase 2 THIO-101 trial (NCT05208944)are still receiving treatment. Additionally, lower rates of toxicity were observed with the combination therapy vs standard-of-care treatment.
"Our longest treated patient so far has completed 21 cycles of THIO sequenced with a [checkpoint inhibitor], and 6 patients who have crossed the 12-month survival follow-up are continuing the treatment," said Vlad Vitoc, MD, chairman and chief executive officer at MAIA, in a press release on treatment updates for the THIO-101 trial.1 "With current therapies, second-line patients’ treatment duration is usually around 3 to 4 months and third-line [therapy] is even lower than that. It is very encouraging to see that our patients can remain on treatment for much longer. The ongoing benefits of THIO in longer-term patients are particularly notable, signifying THIO’s potential as a durable and efficacious treatment for [patients with] advanced NSCLC [who have] limited options."
The dose-optimization phase 2 study recruited adult patients with advanced NSCLC who progressed or relapsed after 1 to 4 prior treatment lines including first-line immune checkpoint inhibitors alone or with platinum chemotherapy.2 An initial safety lead-in cohort included patients receiving 360 mg of THIO intravenously in 120 mg doses over 3 days and 350 mg of intravenous cemiplimab on day 5 of the third week before the stage II design. In the stage I lead-in portion, if 8 or more of 19 patients achieved disease control, 22 patients could be added in that arm, making the total population 41 patients per arm.
According to previous findings presented at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting,prior lines of treatment rates for each arm were 71% for 1 line, 25% for 2 lines, and 4% for 3 lines at the 60 mg dose level and 73% for 1 line, 25% for 2 lines, and 2% for 4 lines at the 180 mg dose level.
Patients in stage II were randomly assigned to receive THIO at either 60 mg, 180 mg, or 360 mg, all followed by cemiplimab treatment every three weeks. Overall, 79 patients received at least 1 dose of THIO as of April 30, 2024. Furthermore, recruitment into the 360 mg arm was halted after an occurrence of grade 4 increase in alanine transaminase (ALT) and aspartate aminotransferase (AST).
Primary end points for the study included dose-limiting toxicities (DLTs), treatment-emergent adverse events (TEAEs), serious AEs, overall response rate (ORR), and disease control rate (DCR).3 Secondary end points included duration of response (DOR), progression-free survival (PFS), and overall survival (OS).
By the stage I cut-off date of November 13, 2023, DCR was 88% in the 60 mg THIO arm and 85% in the 180 mg arm, exceeding the required threshold for stage II expansion. Highlighting a 31% partial response rate and a 54% tumor burden reduction, the trial’s Safety Review Committee selected the 180 mg dose for further investigation due to comparatively higher efficacy with the 60 mg dose.
Most AEs among the treatment population (n = 79) were grades 1 or 2. AST increase (25.3%), ALT increase (21.5%), and nausea (11.4%) were the most common TEAEs. Any LFT elevation instances resolved to baseline and exhibited no clinical symptoms.
References
- MAIA Biotechnology announces new updates from phase 2 trial of novel cancer treatment agent. MAIA Biotechnology. Published July 23, 2024. Accessed July 23, 2024. https://tinyurl.com/5fd6mdbc
- Jankowski T, Csőszi T, Urban L, et al. A phase 2, multicenter, open-label, dose-optimization study evaluating telomere-targeting agent THIO sequenced with cemiplimab in patients with advanced NSCLC: updated results. J Clin Oncol. 2024;42(suppl 16):8601. doi:10.1200/JCO.2024.42.16_suppl.8601
- THIO sequenced with cemiplimab in advanced NSCLC. ClinicalTrials.gov. Updated August 31, 2023. Accessed July 23, 2024. https://clinicaltrials.gov/study/NCT05208944