Tislelizumab Yields Comparable OS, Improves Responses Vs Sorafenib in HCC
Data from the phase 3 RATIONALE-301 trial appear to support tislelizumab as a potential frontline treatment option for patients with unresectable hepatocellular carcinoma.
“These findings demonstrate that tislelizumab represents a potential first-line treatment option for patients with unresectable HCC,” according to the authors of the phase 3 RATIONALE-301 trial (NCT03412773).
Treatment with tislelizumab produced noninferior overall survival (OS) and improvements in objective response rate (ORR) and safety compared with sorafenib tosylate among patients with unresectable hepatocellular carcinoma (HCC), according to findings from the phase 3 RATIONALE-301 trial (NCT03412773) published in JAMA Oncology.
The median OS was 15.9 months (95% CI, 13.2-19.7) among patients receiving tislelizumab vs 14.1 months (95% CI, 12.6-17.4) among those treated with sorafenib, meeting the trial’s primary end point of OS noninferiority with the experimental agent in the intent-to-treat (ITT) population (HR, 0.85; 95.003% CI, 0.71-1.02). In the tislelizumab and sorafenib arms, respectively, the OS rate was 39.0% vs 31.8% at 24 months and 29.2% vs 20.3% at 36 months. Investigators reported that OS findings in the overall population were comparable with those observed across all patient subgroups.
Patients receiving tislelizumab experienced a confirmed ORR of 14.3% compared with 5.4% among patients in the sorafenib arm. Additionally, the median duration of response (DOR) was 36.1 months (95% CI, 16.8-not evaluable [NE]) and 11.0 months (95% CI, 6.2-14.7), and the median time to response was 2.2 months vs 4.0 months in each respective arm. Investigators also reported a disease control rate (DCR) of 44.2% vs 50.3% in each group.
The median progression-free survival (PFS) among patients treated with tislelizumab was 2.1 months (95% CI, 2.1-3.5) compared with 3.4 months (95% CI, 2.2-4.1) among those who received sorafenib (HR, 1.11; 95% CI, 0.92-1.33). The 6-month PFS rate was 28.8% with tislelizumab vs 35.8% with sorafenib. Additionally, the PFS rate in each respective arm was 19.0% vs 18.1% at 12 months, 16.1% vs 9.5% at 18 months, and 13.9% vs 6.1% at 24 months.
“These findings demonstrate that tislelizumab represents a potential first-line treatment option for patients with unresectable HCC,” the study authors wrote.
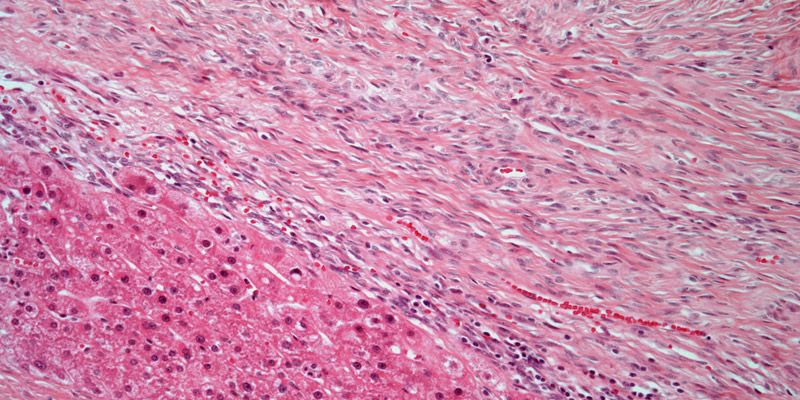
Investigators of the open-label, international phase 3 RATIONALE-301 trial randomly assigned adult patients with histologically confirmed HCC 1:1 to receive 200 mg of tislelizumab intravenously every 3 weeks or 400 mg of sorafenib orally twice a day until disease progression, unacceptable toxicity, or patient withdrawal.
The trial’s secondary end points included ORR, PFS, DOR, DCR, and clinical benefit rate as assessed by blinded independent review committee based on RECIST v1.1 criteria.
Patients 18 years and older with Barcelona Clinic Liver Cancer stage C or B disease not amenable to locoregional therapy or curative treatment were able to enroll on the trial. Additional eligibility criteria included having an ECOG performance status of 0 or 1, Child-Pugh class A liver function, and at least 1 measurable lesion per RECIST v1.1 guidelines.
The analysis set consisted of 674 patients, including 342 of those assigned to treatment with tislelizumab and 332 assigned to receive sorafenib. The median patient age was 61 years (range, 23-86). In the tislelizumab and sorafenib arms, respectively, most patients were male (84.5% and 84.6%) and from Asia (62.9% and 63.3%). Additionally, most patients in each arm had hepatitis B virus only (59.4% and 62.0%), a Child-Pugh score of 5 (76.9% and 74.7%) at study entry, and metastases located in the lung (35.1% and 31.9%).
In the tislelizumab and sorafenib arm, respectively, any-grade treatment-emergent adverse effects (TEAEs) affected 96.2% and 100.0% of patients, and grade 3 or higher TEAEs occurred in 48.2% and 65.4%. Additionally, any-grade treatment-related AEs (TRAEs) were reported in 76.6% and 96.0% of patients, and grade 3 or higher treatment-related toxicities occurred in 22.2% and 53.4%, respectively. Common TRAEs in each arm included aspartate aminotransferase level increases (23.1% and 28.7%), alanine aminotransferase increases (16.6% and 25.0%), and blood bilirubin level increases (12.4% and 20.7%).
Overall, 10.9% of patients discontinued treatment with tislelizumab compared with 18.5% of patients in the sorafenib arm due to TEAEs. Additionally, 6.2% and 10.2% of patients in each respective arm experienced TRAEs that led to treatment discontinuation. Investigators reported TEAEs and TRAEs, respectively, leading to death in 4.4% and 0.9% of patients in the tislelizumab arm and 5.2% and 0.6% of those who received sorafenib.
Reference
Qin S, Kudo M, Meyer T, et al. Tislelizumab vs sorafenib as first-line treatment for unresectable hepatocellular carcinoma: a phase 3 randomized clinical trial. JAMA Oncol. Published online October 5, 2023. doi:10.1001/jamaoncol.2023.4003
Adapting to a Robotic Workstation for Image-Guided Liver Cancer Surgery
December 4th 2023Govindarajan Narayanan, MD, speaks to the potential time-saving advantages of using the Epione robot for microwave ablation, cryoablation, and other surgical strategies in patients with liver cancer and other tumors.