Total Resection Associated With Better Survival in Atypical, Malignant Meningioma
Gross total resection was associated with significantly lower all-cause mortality in patients with atypical and malignant meningioma, according to a new study.
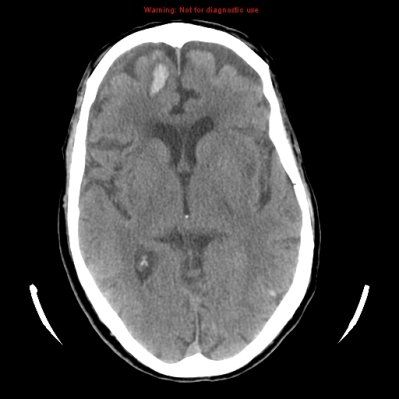
CT scan of a meningioma
Gross total resection (GTR) was associated with significantly lower all-cause mortality in patients with atypical and malignant meningioma, according to a new study.
“Although the prognosis for patients with benign meningioma (WHO grade I) is generally favorable, outcomes for patients with atypical (WHO grade II) and malignant (WHO grade III) meningioma are poor,” wrote study authors led by Ayal A. Aizer, MD, of Brigham and Women’s Hospital in Boston. The extent of resection is known to affect rates of disease progression, but no data previously existed on its connection to overall survival.
The researchers identified 575 atypical and 64 malignant meningioma patients from the SEER database who were diagnosed between 2004 and 2009. Results of the analysis were published online ahead of print in Cancer.
In the atypical meningioma patients, 272 underwent GTR and 303 underwent subtotal resection. In the malignant group, there were 35 GTR patients and 29 subtotal resection patients.
Atypical patients who underwent GTR had a 5-year overall survival rate of 91.3%, compared with only 78.2% in subtotal resection patients. On multivariate analysis, this difference yielded a hazard ratio (HR) of 0.39 (95% CI, 0.23–0.67; P < .001). Increasing age and tumor size were also found to be significantly associated with all-cause mortality.
With regard to malignant meningioma patients, the 5-year overall survival rate for GTR patients was 64.5%, compared with 41.1% for subtotal resection patients. On multivariate analysis this was again significant, with an HR for mortality of 0.35 (95% CI, 0.15–0.81; P = .01). In these patients, older age, larger tumor, and nonwhite race were also adverse prognostic factors.
“In our multivariate models, the association between GTR and survival was profound,” the authors wrote. “Notably, it has been suggested that aggressive removal of malignant meningioma is associated with a higher incidence of morbidity, which may affect overall survival. However, the magnitude of the hazard ratios describing the association between all-cause mortality and the extent of resection in our study suggests that achieving GTR in patients with atypical and malignant meningiomas may be beneficial.”
The authors did note several limitations, including a lack of detail on radiation therapy, performance status, comorbidities, and other factors; these were not available in the SEER database. The study also cannot answer the question of whether more aggressive resection of the tumor in subtotal resection patients would have been beneficial or not, given the potential for increased surgical morbidity.