Treatment With Ibrutinib Plus or Minus Rituximab Associated With Significantly Lower Monthly Cost vs Chemoimmunotherapy in R/R MCL
Treatment with ibrutinib with or without rituximab was associated with a lower monthly health care cost compared with chemoimmunotherapy in a population of patients with relapsed/refractory mantle cell lymphoma.
Patients with relapsed/refractory mantle cell lymphoma (MCL) who were treated with ibrutinib (Imbruvica) with or without rituximab (Rituxan) experienced notably fewer days of outpatient services, as well as a lower monthly total health care cost vs those who received chemoimmunotherapy, according to the results of a real-world retrospective study.1
Findings from the trial indicated that during the first Oncology Care Model (OCM) episode, the number of days with outpatient services per patient per month was significantly lower in the ibrutinib cohort vs the chemoimmunotherapy cohort (rate ratios [RR], 0.63; P< .001). Investigators reported this was driven by a lower number of days with antineoplastic drug administration, as well as less days with outpatient services related to the administration of antineoplastic drugs and fewer days with other outpatient services.
Investigators compared health care resource utilization (HRU) and costs between the 2 groups in the second-line setting (n = 300), including 149 patients in the ibrutinib cohort and 151 in the chemoimmunotherapy cohort. Investigators noted that during the OCM episode and index line of therapy (LOT), the ibrutinib cohort spent significantly less days of the month with outpatient services vs those who received chemoimmunotherapy (OCM, RR = 0.63; P <.001; index LOT, RR = .73; P = .004).
Additionally, within the ibrutinib group, investigators noted a lower mean total monthly all-cause health care cost, as well as lower mean monthly medical costs that worked to fully offset higher mean pharmacy costs per month compared with the chemoimmunotherapy group (P <.001). These lower costs are thought to be driven by lower outpatient costs due to lower costs for antineoplastic drugs and administration. The ibrutinib cohort was also found to have significantly lower overall monthly health care costs, as well.
“Among patients with [relapsed/refractory] MCL, monthly HRU and total all-cause health care costs from the payer's perspective were significantly lower among those receiving [ibrutinib with/without rituximab] compared to [chemoimmunotherapy], with monthly medical cost-savings fully offsetting higher monthly pharmacy costs,” the authors of the study wrote. “This result was consistent with those from the evaluation of HRU and health care costs during the first OCM episode following the initiation of the index regimen and the observed duration of the index LOT.”
The study utilized data that was collected between May 13, 2013, and June 30, 2019, from Optum’s de-identified Clinformatics Data Mart database. Investigators included 2 stages in the study, with stage 1 utilizing a retrospective design to evaluate the treatment of patients in the first line and the second stage using the same design to compare HRU and healthcare costs between those treated with ibrutinib and chemoimmunotherapy in the second-line setting.
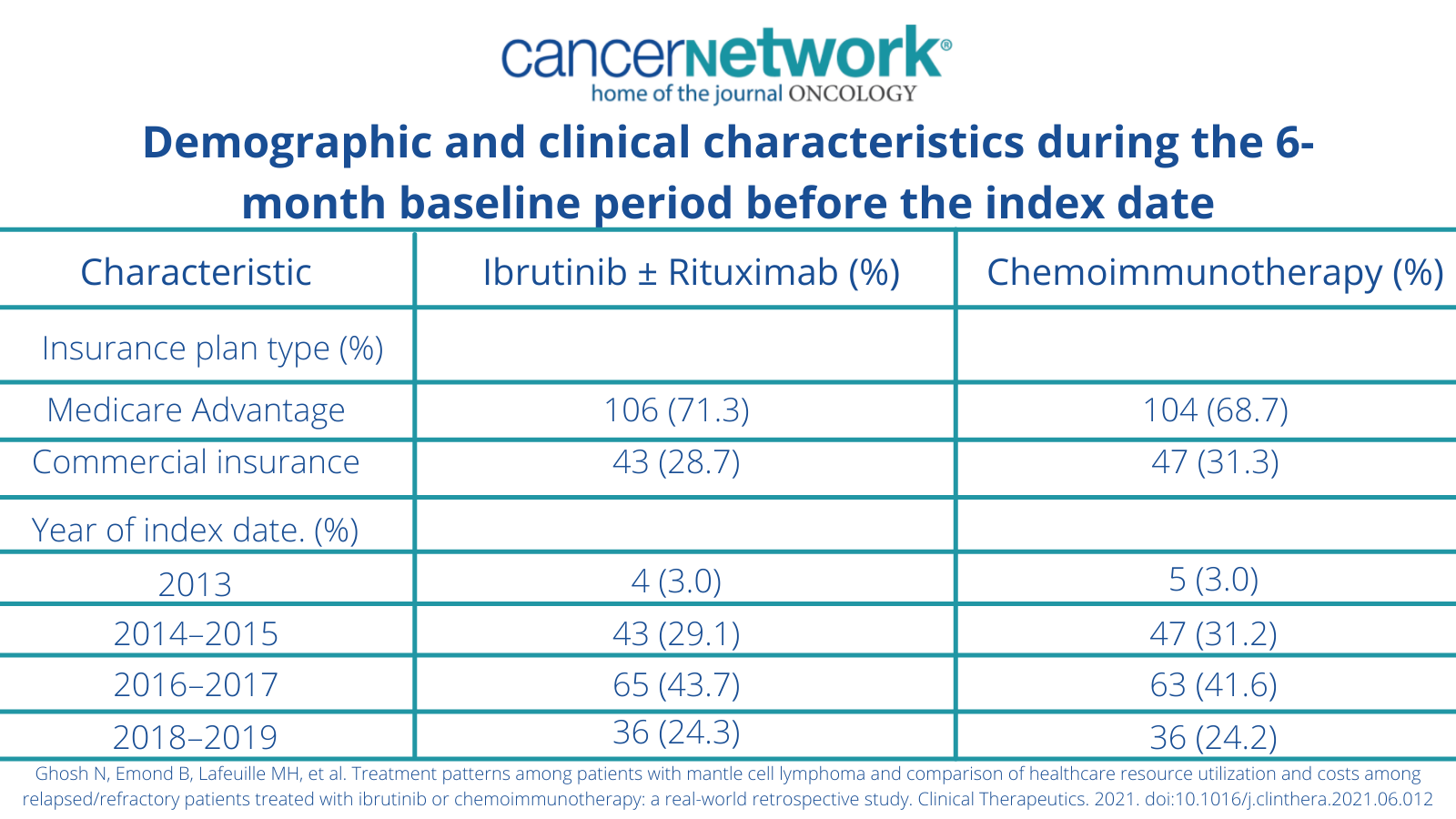
Demographic and clinical characteristics during the 6-month baseline period before the index date
Before beginning treatment with either ibrutinib or chemoimmunotherapy, patients needed to have undergone an initial treatment such as antineoplastic therapy or hematopoietic stem cell transplant (HSCT). To be included in the second part of the study, patients needed to have 2 or more claims with a diagnosis for MCL at any time and initiated a second observed regimen after their first regimen or HSCT. Patients then needed to initiate treatment with either ibrutinib with or without rituximab or chemoimmunotherapy with HSCT as a second-line therapy.
In total, 1346 patients were included in the study at a median follow-up of 15.3 months.
“The findings from the present study also suggest that HRU and costs should be taken into account, in addition to efficacy and safety, when establishing optimal treatment sequencing with novel targeted therapies such as ibrutinib among patients with [relapsed/refractory] MCL, as they may be useful in improving patients' care,” the authors concluded.
References
Ghosh N, Emond B, Lafeuille MH, et al. Treatment patterns among patients with mantle cell lymphoma and comparison of healthcare resource utilization and costs among relapsed/refractory patients treated with ibrutinib or chemoimmunotherapy: a real-world retrospective study. Clinical Therapeutics. 2021. doi:10.1016/j.clinthera.2021.06.012
Highlighting Insights From the Marginal Zone Lymphoma Workshop
Clinicians outline the significance of the MZL Workshop, where a gathering of international experts in the field discussed updates in the disease state.