Uterine sarcomas are rare malignant uterine neoplasms that are responsible for a large majority of uterine cancer–associated deaths. The subtypes include leiomyosarcomas, endometrial stromal tumors, and adenosarcomas. Standard treatment includes complete surgical resection. Adjuvant treatment with chemotherapy, hormonal therapy, or radiation may be considered in patients with high-risk disease. However, because the ability of adjuvant treatment to improve overall survival in patients with uterine sarcomas is unclear, there is no standard recommendation regarding adjuvant therapy. The risk in forgoing chemotherapy is that uterine sarcomas have a tendency to develop distant recurrences. Many cytotoxic agents have been investigated in clinical trials in an attempt to identify an effective treatment that can improve the course of this disease. Adjuvant radiation appears to improve local control but has no significant impact on survival. In this review we discuss preoperative diagnosis and the role of pathology, and we summarize the current literature regarding the management of uterine sarcomas.
Introduction
Malignant mesenchymal tumors of the uterine corpus are rare tumors. They comprise less than 3% of all uterine corpus tumors,[1] yet account for a disproportionate percentage of deaths from uterine cancers. In one series, the mortality rate from uterine sarcomas was reported to be as high as 29%.[2] Survival is dependent on stage; the estimated 5-year survival rate for stage I uterine leiomyosarcoma is 76%, while it is 60% for stage II, 45% for stage III, and 29% for stage IV disease.[3]
Historically, uterine sarcomas have been grouped together for the purposes of clinical trials. While this has aided accrual, the heterogeneous behavior of these tumors has limited clinical applicability of the trial results. The World Health Organization (WHO) has published a classification system based on the differentiation and growth pattern, and on the cell of origin.[4] There are two main groups of uterine sarcomas in the WHO classification system: mesenchymal tumors, and mixed epithelial and mesenchymal tumors. The former group includes leiomyosarcomas, endometrial stromal sarcomas, undifferentiated endometrial sarcomas, and smooth muscle tumors of uncertain malignant potential; and the latter group includes carcinosarcomas, Müllerian adenosarcomas, carcinofibromas, adenofibromas, and adenomyomas. Uterine carcinosarcoma, previously known as “mixed mesodermal tumor” and classified as a uterine sarcoma, is now widely believed to be a metaplastic, high-grade endometrial adenocarcinoma; we will cover these tumors briefly.
Leiomyosarcomas are the most common uterine sarcomas, followed by endometrial stromal sarcomas, undifferentiated endometrial sarcomas, and Müllerian adenosarcomas. Still, these are all rare tumors: a recent study using Scandinavian databases found an incidence rate for leiomyosarcoma of 0.4 per 100,000 women, and an incidence rate for endometrial stromal sarcomas of 0.3 per 100,000 women. Over the study period of 1978 to 1997, the incidence rates of both diseases were constant.[5]
Generally, patients do not have identifiable risk factors; however, there are germline mutations, including p53 and Rb, that are associated with an increased risk for leiomyosarcoma and other cancers.[6,7] Also, some studies suggest an increased risk for uterine sarcoma in women with a history of obesity, diabetes mellitus, younger age at menarche, or exposure to tamoxifen.[8,9]
Preoperative diagnosis of uterine sarcoma is often difficult. Women with early-stage uterine sarcoma will present with the same set of symptoms associated with the much more common uterine leiomyomata; these include postmenopausal bleeding, abnormal uterine bleeding, abdominal or pelvic pain and/or pressure, bloating or distention, constipation, enlarging abdomen, urinary symptoms, and abnormal or foul-smelling vaginal discharge. Some women are asymptomatic.
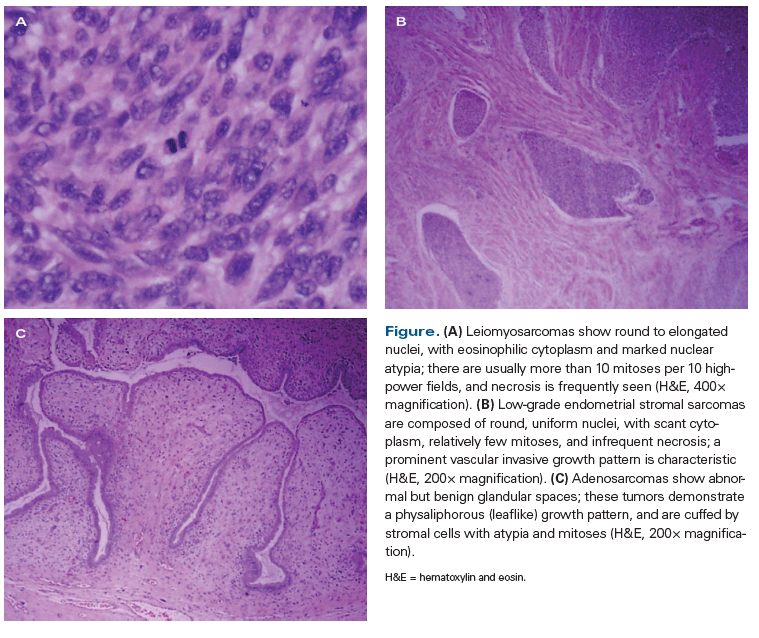
Because presenting symptoms may be vague and because optimal treatment of sarcoma is dependent on an accurate and precise diagnosis, seeking the assistance of a multidisciplinary team may be warranted. To ensure proper assessment prior to treatment, such a team should include a gynecologic oncologist, a medical oncologist, radiologists, and pathologists. Newer radiologic techniques may assist in confirming suspicion of a malignancy. In addition, careful histologic review is critical; since the different sarcoma histologic subtypes vary in prognosis and management, expert review by a gynecologic pathologist or sarcoma pathologist is recommended (Figure).
Endometrial sampling is considered a standard preoperative diagnostic test in uterine neoplasms. However, since uterine sarcomas originate in the myometrium, performance of endometrial biopsies has a low predictive value for identification of uterine sarcomas.[10] Some investigators have examined the utility of needle biopsy as a preoperative diagnostic test. A recent study involving 63 patients with inconclusive MRI who underwent needle biopsy demonstrated sensitivity, specificity, and positive and negative predictive values for the procedure of 91.7%, 100%, 100%, and 96.2%, respectively.[11]
Imaging with ultrasound, CT, or MRI may identify a uterine mass. Unfortunately, no imaging modality has been shown to accurately differentiate between leiomyomatas and uterine sarcomas. However, novel techniques that use diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) values are beginning to be used to assist in classifying patients into two groups: those with low-risk disease that is likely benign, and those with high-risk disease in whom there is a possibility of leiomyosarcoma.[12,13] In general, intermediate to high signal on DWI and low ADC values are correlated with malignant lesions. Uterine masses that continue to increase in size after menopause should also be concerning for malignancy. In addition to MRI, serum lactate dehydrogenase (LDH) isoenzyme levels, particularly an elevation of LDH isoenzyme type 3, may be useful in making a diagnosis of leiomyosarcoma.[14]
Whenever possible, surgery should be undertaken in patients with uterine sarcoma in order to remove all sites of disease and for purposes of accurate staging. It is prudent to have a gynecologic oncologist or surgical oncologist perform surgical staging if possible. In 2009, the International Federation of Gynecology and Obstetrics (FIGO) released a staging system specific for uterine sarcomas. This system actually comprises two distinct staging systems: one for leiomyosarcoma and endometrial stromal sarcoma, and another for adenosarcoma. Carcinosarcomas should be staged using the endometrial cancer staging system. The extent of the surgery depends on the histologic subtype.
Leiomyosarcoma
Surgery
As described in the National Comprehensive Cancer Network (NCCN) guidelines,[15] an initial diagnosis is made after a first intervention (hysterectomy, myomectomy, or biopsy). Following expert pathologic review of the specimen, a determination is made as to whether the patient should undergo additional surgery, or, if the patient is not a surgical candidate, the type of primary treatment (radiation or systemic therapy) that should be initiated. In most cases, surgery-if feasible-is the preferred initial management.
For patients with early-stage leiomyosarcoma, surgical management consists of total hysterectomy and surgical cytoreduction of intra-abdominal and retroperitoneal disease. Normal-appearing lymph nodes are unlikely to be involved, making routine lymphadenectomy unnecessary; only suspicious lymph nodes should be removed.[16-18] Most surgeons perform a bilateral salpingo-oophorectomy at the time of total hysterectomy, particularly in perimenopausal and postmenopausal women. However, it is not clear whether bilateral salpingo-oophorectomy influences the survival of patients with newly diagnosed leiomyosarcoma. A Surveillance, Epidemiology, and End Results (SEER) study by Kapp et al that included over 1,300 women showed no survival advantage in women under the age of 50 with leiomyosarcoma who had their ovaries removed, nor in those who did not have their ovaries removed.[3]
In patients who have locally advanced disease or limited metastatic disease, an attempt to resect all disease is reasonable and may improve survival. In one series, women whose disease was completely resected had a 12-month improvement in overall survival (OS) compared with those with residual disease.[19] A study of women undergoing pulmonary metastasectomy for metastases from leiomyosarcoma showed a median OS of 70 months.[20]
The widespread use of minimally invasive surgical techniques for leiomyomata, including power morcellation, has led to increasing concern about the possibility of inadvertent anatomic disruption of undiagnosed leiomyosarcoma. Several studies demonstrate that patients who undergo morcellation for presumed benign disease, and who are subsequently diagnosed with leiomyosarcoma, have worse outcomes compared with women who undergo hysterectomy.[21-23] Power morcellation is associated with an increased risk of tumor recurrence, likely due to fragmentation and spread of leiomyosarcoma in the intraperitoneal cavity. For women who have undergone myomectomy for what was presumed to be leiomyomata, completion hysterectomy is indicated if high-grade leiomyosarcoma is discovered. In one report, two-thirds of patients had residual disease at completion hysterectomy.[24]
Adjuvant therapy
Pelvic radiation. Stage I and II leiomyosarcomas have a 50% to 70% risk of recurrence, with more than half of recurrences being extrapelvic recurrences that are often multisite and lethal.[25-27] The use of adjuvant pelvic radiation therapy (RT) has been debated, with the majority of the literature addressing the question limited to retrospective reviews. Despite the bias inherent in retrospective studies, these have shown that adjuvant RT yields improved local control of disease; however, likely because of distant spread, they have not demonstrated a change in OS.[28-30]
The European Organisation for Research and Treatment of Cancer (EORTC) protocol 55874 evaluated the role of adjuvant RT in patients with stage I or II uterine sarcoma.[31] Patients were randomly assigned to either observation or pelvic RT after undergoing a minimum surgery of hysterectomy, bilateral salpingo-oophorectomy, and pelvic washings. Of the 224 patients accrued, 103 had leiomyosarcoma histology. As expected, there was improvement in local control overall, but no improvement in OS. A subgroup analysis of the leiomyosarcoma patients showed no benefit from RT in achieving either local control or OS. A SEER analysis that included 1,088 patients with leiomyosarcoma also concluded that adjuvant RT had no survival benefit in this population.[32]
Chemotherapy. Adjuvant chemotherapy is undertaken with the hope that it will have an effect on micrometastases and will improve outcomes for the many patients likely to develop distant disease. For stage I and II leiomyosarcoma, studies have not shown a survival benefit for adjuvant chemotherapy.[27] Mancari et al examined 140 patients with leiomyosarcoma, 37% of whom received chemotherapy and 44% of whom were observed postoperatively. The median survival after relapse was 20 months for the chemotherapy group compared with 28 months for the observation group.[33]
The phase III Gynecologic Oncology Group (GOG) 20 randomized controlled trial compared doxorubicin vs observation in patients with stage II uterine sarcoma, including carcinosarcoma and leiomyosarcoma. Physicians were allowed to use external beam RT prior to the randomization to chemotherapy or observation. Despite a 9-year accrual, only 156 patients were evaluable, 48 with leiomyosarcoma. There was no difference in OS or progression-free survival (PFS) between the two groups.[34] No statistical difference was seen in the leiomyosarcoma patients, with recurrence noted in 44% (11/25) in the doxorubicin arm vs 61% (14/23) in the observation arm. The addition of doxorubicin did not have an impact on PFS or OS. However, the limited accrual and other study limitations, including multiple protocol violations, would have made it unlikely for any results to have been practice-changing.
Due to its activity in recurrent/metastatic disease, the combination of fixed-dose-rate gemcitabine plus docetaxel, followed by doxorubicin, was evaluated in Sarcoma Alliance for Research through Collaboration (SARC) protocol 005 as adjuvant therapy for resected stage I and II leiomyosarcoma.[35] Median follow-up was 39.8 months, with 46% of patients developing recurrent disease. Seventy-eight percent of patients were progression-free at 2 years, and 57% were progression-free at 3 years. These results are promising compared with historical controls. We are now awaiting the results of a prospective phase III trial comparing this regimen with observation (ClinicalTrials.gov identifier: NCT01533207).
Treatment of advanced and recurrent leiomyosarcoma
Metastatic or recurrent disease is most commonly seen in the abdomen; distant extra-abdominal metastases are most often found in the lungs, bone, liver, and central nervous system. For patients undergoing surveillance following treatment of a primary leiomyosarcoma, NCCN guidelines recommend physical examination every 3 months for 2 years, then every 6 to 12 months; and CT scans of the chest, abdomen, and pelvis every 6 months for the first 3 years, then every 6 to 12 months for the following 2 years.[15] Imaging should also be considered based on symptomatology and clinical concern for recurrence or metastatic disease. When recurrence or metastasis occurs, surgical resection should be considered, and complete resection should be performed if it is possible to do this with minimal morbidity, since there are few effective systemic treatment options.
Several studies have reported successful intervention with metastasectomy for patients with leiomyosarcoma, particularly in cases of lung metastasis.[19,20,36] Both primary and secondary cytoreductive surgery have been reported to be associated with a prolonged progression-free interval and prolonged survival.[19,37]
Adjuvant RT. Currently, there are no randomized phase III trials that show adjuvant RT to have an impact on survival or chance of relapse in patients with advanced or recurrent leiomyosarcoma. The role of radiation in patients with advanced or recurrent disease is to palliate tumor-associated symptoms. In patients in whom surgical resection is not an option, RT may be used to decrease the tumor burden and reduce bleeding, obstruction, and/or pain. The approach to palliative RT is described in Radiation Therapy Oncology Group (RTOG) 8502. In this study in patients with advanced pelvic malignancies (39.4% of which were gynecologic), 44.40 Gy was administered in 12 fractions (3.7 Gy twice daily), with two treatment breaks.[38,39] Six percent of patients developed grade 3 or higher late toxicities.[39]
Adjuvant chemotherapy. Chemotherapy for patients with recurrent or metastatic leiomyosarcoma is usually considered palliative. The NCCN guidelines recommend participation in clinical trials in this population as standard of care; however, given the rarity of this disease, there are few trials that are dedicated solely to this patient population.[15] Patients who are referred to sarcoma centers are enrolled in more clinical trials and have a median OS advantage of 2.07 years compared with patients who are just followed by gynecologic oncologists.[40] The goals of treatment in patients with recurrent or metastatic disease are to relieve symptoms and extend time to progression. It is important for patients to comprehend the palliative nature of their treatment, and it is reasonable to offer best supportive care in this setting.
Initial trials of chemotherapy in recurrent disease were conducted without separation of the various sarcoma subtypes. Omura et al compared doxorubicin with and without dacarbazine in the treatment of stage III or IV and recurrent uterine sarcomas. Doxorubicin alone had a 16% response rate (RR), while the RR with the combination therapy was 24%. There was no survival advantage for either regimen, but patients with leiomyosarcoma histology had a significantly longer survival than patients with other histologies.[41] Nevertheless, doxorubicin-based therapy was considered first-line therapy for metastatic unresectable sarcomas, including leiomyosarcoma. Other agents with moderate activity include ifosfamide (RR, 17%), gemcitabine (RR, 20%), liposomal doxorubicin (RR, 16.1%), and trabectedin (RR, 8% to 10%).[42-46]
In 2008, Hensley et al demonstrated that fixed-dose-rate gemcitabine plus docetaxel achieved high objective RRs as first-line treatment for metastatic disease.[47] Patients with advanced unresectable uterine leiomyosarcoma, with measurable disease and without a history of pelvic RT or chemotherapy, were eligible. They received gemcitabine 900 mg/m2 on days 2 and 8, followed by docetaxel 100 mg/m2 on day 8. Granulocyte colony-stimulating factor was given following chemotherapy as part of the treatment regimen. Of the 42 patients included in this study, 15 had measurable objective responses, for a 35.8% overall RR (4.8% with complete responses, 31% with partial responses). The most common grade 3 or higher toxicities were myelosuppression and fatigue. The addition of bevacizumab to this regimen did not improve PFS, objective responses, or overall RR.[48] Thus, the combination of gemcitabine and docetaxel is the standard first-line treatment for advanced or metastatic disease.
The combination regimen of gemcitabine and docetaxel has also been evaluated as a second-line treatment. The French Sarcoma Group TAXOGEM study was a randomized, multicenter, phase II trial evaluating single-agent gemcitabine vs gemcitabine plus docetaxel as second-line treatment for metastatic or unresectable leiomyosarcoma after a prior anthracycline-based regimen. Patients with nonuterine leiomyosarcoma as well as those with disease of uterine origin were included, and a secondary analysis was performed in all patients. Gemcitabine 1,000 mg/m2 was administered on days 1, 8, and 15 of a 28-day cycle in those who received single-agent therapy. The regimen in the doublet arm consisted of gemcitabine 900 mg/m2 on days 1 and 8 plus docetaxel 100 mg/m2 on day 8 of a 21-day cycle. Both regimens were found to be effective second-line regimens for leiomyosarcoma, but the combination treatment was not superior to gemcitabine alone: the 3-month PFS rate for both drug regimens was 40%, regardless of whether disease had a uterine or nonuterine site of origin. Also, patients who received single-agent gemcitabine experienced less toxicity.[49]
Another combination treatment, trabectedin and doxorubicin, was evaluated in a phase II trial for patients with advanced disease who had not received any prior chemotherapy. In the 47 patients in the uterine leiomyosarcoma group, the overall RR was 60% and median PFS was 8.2 months. The most common grade 3/4 treatment toxicities included myelosuppression, elevated alanine aminotransferase levels, febrile neutropenia, and fatigue.[50]
The combination treatment of doxorubicin, cisplatin, and ifosfamide (API) was studied at a single institution in patients with metastatic leiomyosarcoma under the age of 65 (median age, 51 years). This study used an aggressive multimodal approach that included API chemotherapy, as well as additional surgery, RT, or radiofrequency ablation therapy, as deemed necessary. The overall RR was 48%, but with significant grade 3/4 toxicities.[51]
KEY POINTS
- Uterine sarcomas are rare tumors that tend to behave more aggressively and that are associated with a poor prognosis.
- Diagnosis is usually made following surgical intervention, which often has been performed for benign reasons.
- The management of uterine sarcomas should employ an interdisciplinary approach.
- Adjuvant treatment with chemotherapy or radiation may be considered after initial surgery; however, it is unclear whether such treatment will improve survival outcomes.
Hormonal therapy. Leiomyosarcomas are reported to express estrogen receptors (ERs) and/or progesterone receptors (PRs) in 40% to 80% of cases.[52,53] Leitao et al showed that PR immunohistochemical expression-but not ER expression-appeared to be associated with improved PFS and OS.[52] However, when adjusted for stage, ER expression was associated with PFS. Aromatase inhibitors are well-tolerated hormonal modulating agents that have been used in postmenopausal women with breast cancer, and their use in patients with leiomyosarcoma has been shown to have some efficacy. A recent single-arm phase II clinical trial that included 27 patients showed that letrozole met the protocol definition of an active agent in metastatic leiomyosarcoma that was ER- and/or PR-positive.[53] Therefore, it is not unreasonable to consider the use of aromatase inhibitors in patients with ER/PR-positive leiomyosarcoma with low disease burden.
Endometrial Stromal Tumors: Low-Grade Endometrial Stromal Sarcomas and Undifferentiated Endometrial Sarcomas
In 2014, the WHO reclassified endometrial stromal tumors into three categories: endometrial stromal nodules, endometrial stromal sarcomas, and undifferentiated endometrial sarcomas.[4] An endometrial stromal nodule is a benign finding and is treated with a simple hysterectomy. The designation of low-grade endometrial stromal sarcoma has been maintained; however, the high-grade endometrial stromal sarcoma classification is now referred to as “undifferentiated endometrial sarcoma.” Most low-grade endometrial stromal sarcomas are hormonally sensitive and generally behave in an indolent manner, with long disease-free intervals.
Surgery is the cornerstone of treatment for low-grade endometrial stromal sarcoma and generally consists of hysterectomy and bilateral salpingo-oophorectomy. Importantly, extensive surgical staging is not necessary and does not have survival benefit. Lymphadenectomy should be limited to patients with bulky nodal disease.[54] These tumors are generally hormonally responsive, and ovarian preservation has been shown to be associated with a higher recurrence rate compared with bilateral salpingo-oophorectomy. For this reason, bilateral salpingo-oophorectomy is generally recommended, although it does not appear to have an impact on OS.[55] Also, a SEER database analysis showed no adverse impact on survival for patients retaining their ovaries.[56] Thus, ovarian-sparing surgeries may be considered in young women. Given the rarity of this disease, using large population-based databases such as the SEER database may provide insights that can help with treatment decisions; still, it is important to recognize the limitations of this approach, particularly of the generalizability of the data.
The benefit of adjuvant therapy is unclear in completely resected early-stage low-grade endometrial stromal sarcoma. In patients with advanced-stage or recurrent disease, hormonal therapy is the primary treatment, since it is well tolerated and has minimal side effects.[57,58] Many studies demonstrate the presence of steroid receptors-for both estrogen and progesterone-in tumors originating from endometrial stromal cells.[59-61] Wade et al showed a 48% rate of ER expression and a 30% rate of PR expression.[59] Treatment of these tumors with aromatase inhibitors and gonadotropin-releasing hormone agonists has shown acceptable long-term outcomes in advanced disease, and these agents are reasonable to use, given their favorable toxicity profiles.[61,62]
Undifferentiated endometrial sarcoma behaves quite differently from low-grade endometrial stromal sarcoma, with a high risk of recurrence regardless of stage and rare responses to chemotherapy. These tumors can be subcategorized into two types: those with monomorphic/uniform nuclei and those with pleomorphic nuclei. The former group is more likely to express hormone receptor positivity than the latter group and appears to be associated with better outcomes.[63] There are only a few studies that evaluate the outcomes of adjuvant treatment in recurrent undifferentiated endometrial sarcoma. A multi-institutional phase II study examined the effectiveness of ifosfamide in this setting and demonstrated a 33% overall RR.[64] There are also reports of other agents that are effective, including doxorubicin, etoposide, and gemcitabine plus docetaxel.[65-67]
Adenosarcoma
Adenosarcomas of the uterus are rare mixed neoplasms composed of a malignant but often low-grade mesenchymal component along with a benign epithelium. They are usually considered low-grade neoplasms that have low malignant potential and a good prognosis. Most patients are diagnosed at an early stage; the 5-year survival rate is 79% for stage I disease.[68] The presence of sarcomatous overgrowth and myometrial invasion together is associated with higher rates of recurrence and poorer prognosis.[69,70] Surgical management includes hysterectomy with bilateral salpingo-oophorectomy. Ovarian preservation may be considered, since it appears to be safe in premenopausal women whose disease has low-risk features.[70] The role of adjuvant therapy is unclear, although it may be considered in cases with high-risk features such as sarcomatous overgrowth or myometrial invasion, given the increased risk of recurrence. There are no data demonstrating an effective response. Other treatment options include RT and hormonal therapy.
Conclusion
The standard treatment for early- and advanced-stage uterine sarcomas is surgical intervention and complete cytoreduction of extrauterine disease. Immunohistologic studies should be performed, since the results may guide adjuvant therapy decisions. In early-stage disease, adjuvant chemotherapy or RT should not be administered routinely, since the benefit of both is unclear. The standard treatment for advanced or recurrent disease is combination gemcitabine and docetaxel, although trabectedin is emerging as a promising agent in the recurrent setting as well. Low-grade endometrial stromal sarcomas are indolent and carry a favorable prognosis. High-grade or undifferentiated endometrial sarcomas are aggressive and have a less favorable prognosis, given that they seldom respond to chemotherapy.
Financial Disclosure:The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Siegel R, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29.
2. Nordal RR, Thoresen SO. Uterine sarcomas in Norway 1956–1992: incidence, survival and mortality. Eur J Cancer. 1997;33:907-11.
3. Kapp DS, Shin JY, Chan JK, et al. Prognostic factors and survival in 1396 patients with uterine leiomyosarcoma: emphasis on impact of lymphadenectomy and oophorectomy. Cancer. 2008;112:820-30.
4. IARC Publications. Pathology and genetics of tumors of the breast and female genital organs. World Health Organization Classification of Tumours. http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb4/. Accessed February 7, 2017.
5. Koivisto-Korander R, Martinsen JI, Weiderpass E, et al. Incidence of uterine leiomyosarcoma and endometrial stromal sarcoma in Nordic countries: results from NORDCAN and NOCCA databases. Maturitas. 2012;72:56-60.
6. Gonzalez KD, Noltner KA, Busin CH, et al. Beyond Li Fraumeni syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol. 2009;8:1250-6.
7. Kleinerman RA, Tucker MA, Tacrone RE, et al. Risk of new cancers after radiotherapy in long term survivors of retinoblastoma: an extended follow-up. J Clin Oncol. 2005;23:2272-9.
8. Felix AS, Cook LS, Gaudet MM, et al. The etiology of uterine sarcomas: a pooled analysis of the epidemiology of endometrial cancer consortium. Br J Cancer. 2013;108:727-34.
9. Lavie O, Barnett-Griss O, Narod SA, et al. The risk of developing uterine sarcoma after tamoxifen use. Int J Gynecol Cancer. 2008;18:352-6.
10. Bansal N, Herzog TJ, Burke W, et al. The utility of preoperative endometrial sampling for the detection of uterine sarcomas. Gynecol Oncol. 2008;110:43-8.
11. Ryo T, Katsunori K, Mina A, et al. Preoperative ultrasound guided needle biopsy of 63 uterine tumors having high signal intensity upon T2 weighted magnetic resonance imaging. Int J Gynecol Cancer. 2014;24:1042-7.
12. Li HM, Liu J, Qiang JW, et al. Diffusion weighted imaging for differentiating uterine leiomyosarcoma from degenerated leiomyoma. J Comput Assist Tomogr. 2016 Dec 15. [Epub ahead of print]
13. Sato K, Yuasa N, Fujita M, et al. Clinical application of diffusion-weighted imaging for preoperative differentiation between uterine leiomyoma and leiomyosarcoma. Am J Obstet Gynecol. 2014;210:368.e1-8.
14. Goto A, Takeuchi S, Sugimura K, Maruo T. Usefulness of Gd-DTPA contrast-enhanced dynamic MRI and serum determination of LDH and its isozymes in the differential diagnosis of leiomyosarcoma from degenerating leiomyoma of the uterus. Int J Gynecol Cancer. 2002;12:354-61.
15. NCCN clinical practice guidelines in oncology (NCCN guidelines®). Uterine neoplasms. Version 1.2017. https://www.nccn.org/professionals/physician_gls/pdf/uterine.pdf. Accessed February 3, 2017.
16. Giuntoli RL, Metzinger DS, DiMarco CS, et al. Retrospective review of 208 patients with leiomyosarcoma of the uterus: prognostic indicators, surgical management, and adjuvant therapy. Gynecol Oncol. 2003;89:460-9.
17. Yamada SD, Burger RA, Brewster WR, et al. Pathologic variables and adjuvant therapy as predictors of recurrence and survival for patients with surgically evaluated carcinosarcoma of the uterus. Cancer. 2000;88:2782-6.
18. Goff BA, Rice LW, Fleischhacker D, et al. Uterine leiomyosarcoma and endometrial stromal sarcoma: lymph node metastases and sites of recurrence. Gynecol Oncol. 1999;50:105-9.
19. Leitao MM, Zivanovic O, Chi D, et al. Surgical cytoreduction in patients with metastatic uterine leiomyosarcoma at the time of initial diagnosis. Gynecol Oncol. 2012;125:409-13.
20. Burt BM, Ocejo S, Mery MC, et al. Repeated and aggressive pulmonary resections for leiomyosarcoma metastases extends survival. Ann Thorac Surg. 2011;92:1202-7.
21. George S, Barysauskas C, Serrano C, et al. Retrospective cohort study evaluating the impact of intraperitoneal morcellation of outcomes of localized uterine leiomyosarcoma. Cancer. 2014;120:3154-8.
22. Park JY, Park SK, Kim DY, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparent early uterine leiomyosarcoma. Gynecol Oncol. 2011;122:255-9.
23. Morice P, Rodriguez A, Rey A, et al. Prognostic value of initial surgical procedure for patients with uterine sarcoma: analysis of 123 patients. Eur J Gynaecol Oncol. 2003;24:237-40.
24. Berchuck A, Rubin SC, Hoskins WJ, et al. Treatment of uterine leiomyosarcoma. Obstet Gynecol. 1988;71:845-50.
25. Major FJ, Blessing JA, Silverberg SG, et al. Prognostic factors in early-stage uterine sarcoma. A Gynecologic Oncology Group study. Cancer. 1993;71:1702-9.
26. Gadducci A, Landoni F, Sartori E, et al. Uterine leiomyosarcoma: analysis of treatment failures and survival. Gynecol Oncol. 1996;62:25-32.
27. Ricci S, Giuntoli RL 2nd, Eisenhauer E, et al. Does adjuvant chemotherapy improve survival for women with early-stage uterine leiomyosarcoma? Gynecol Oncol. 2013;131:629-33.
28. Salazar OM, Bonfiglio TA, Patten SE, et al. Uterine sarcomas: analysis of failures with special emphasis on the use of adjuvant radiation therapy. Cancer. 1978;42:1161-70.
29. Knocke TH, Kucera H, Dorfler D, et al. Results of postoperative radiotherapy in the treatment of sarcoma of the corpus uteri. Cancer. 1998;83:1972-9.
30. Sorbe B. Radiotherapy and/or chemotherapy as adjuvant therapy of uterine sarcomas. Gynecol Oncol. 1985;20:281-9.
31. Reed NS, Mangioni C, Malmstrom H, et al. Phase III randomized study to evaluate the role of adjuvant pelvic radiotherapy in the treatment of uterine sarcomas stages I and II: a European Organisation for Research and Treatment of Cancer Gynaecological Cancer Group Study (protocol 55874). Eur J Cancer. 2008;44:808-18.
32. Wright JD, Seshan VE, Shah M, et al. The role of radiation in improving survival for early stage carcinosarcoma and leiomyosarcoma. Am J Obstet Gynecol. 2008;199:536.e1-8.
33. Mancari R, Signorelli M, Gadducci A, et al. Adjuvant chemotherapy in stage I–II uterine leiomyosarcoma: a multicentric retrospective study of 140 patients. Gynecol Oncol. 2014;133:531-6.
34. Omura GA, Blessing JA, Major F, et al. A randomized clinical trial of adjuvant adriamycin in uterine sarcomas: a Gynecologic Oncology Group study. J Clin Oncol. 1985;3:1240-5.
35. Hensley ML, Wathen JK, Maki RG, et al. Adjuvant therapy for high-grade, uterus-limited leiomyosarcoma: results of a phase 2 trial (SARC 005). Cancer. 2013;119:1555-61.
36. Clavero JM, Deschamps C, Cassivi SD, et al. Gynecologic cancers: factors affecting survival after pulmonary metastasectomy. Ann Thorac Surg. 2006;81:2004-7.
37. Giuntoli RL, Garrett-Mayer E, Bristow RE, et al. Secondary cytoreduction in the management of recurrent uterine leiomyosarcoma. Gynecol Oncol. 2007;106:82-8.
38. Spanos W Jr, Guse C, Perez C, et al. Phase II study of multiple daily fractionations in the palliation of advanced pelvic malignancies: preliminary report of RTOG 8502. Int J Radiat Oncol Biol Phys. 1989;17:659-61.
39. Spanos WJ Jr, Clery M, Perez CA, et al. Late effect of multiple daily fraction palliation schedule for advanced pelvic malignancies (RTOG 8502). Int J Radiat Oncol Biol Phys. 1994;29:961-7.
40. Lange SE, Liu J, Adkins DR, et al. Improved clinical trial enrollments for uterine leiomyosarcoma patients after gynecologic oncology partnership with a sarcoma center. Gynecol Oncol. 2016;140:307-12.
41. Omura GA, Major FJ, Blessing JA, et al. A randomized study of adriamycin with and without dimethyl triazenoimidazole carboxamide in advanced uterine sarcomas. Cancer. 1983;52:626-32.
42. Sutton GP, Blessing JA, Rosenshein N, et al. Phase II trial of ifosfamide and mesna in mixed mesodermal tumors of the uterus: a Gynecologic Oncology Group study. Am J Obstet Gynecol. 1989;161:309-12.
43. Look KY, Sandler A, Blessing JA, et al. Phase II trial of gemcitabine as second-line chemotherapy of uterine leiomyosarcoma: a Gynecologic Oncology Group (GOG) study. Gynecol Oncol. 2004;92:644-7.
44. Garcia-Carbonero R, Supko JG, Manola J, et al. Phase II and pharmacokinetic study of ecteinascidin 743 in patients with progressive sarcomas of soft tissues refractory to chemotherapy. J Clin Oncol. 2004;22:1480-90.
45. Sutton G, Blessing J, Hanjani P, et al. Phase II evaluation of liposomal doxorubicin (Doxil) in recurrent or advanced leiomyosarcoma of the uterus: a Gynecologic Oncology Group study. Gynecol Oncol. 2005;96:749-52.
46. Demetri GD, von Mehren M, Jones RL, et al. Efficacy and safety of trabectedin or dacarbazine for metastatic liposarcoma or leiomyosarcoma after failure of conventional chemotherapy: results of a phase III randomized multicenter clinical trial. J Clin Oncol. 2016;34:786-93.
47. Hensley ML, Blessing JA, Mannel R, et al. Fixed-dose rate gemcitabine plus docetaxel as first-line therapy for metastatic uterine leiomyosarcoma: a Gynecologic Oncology Group phase II trial. Gynecol Oncol. 2008;109:329-34.
48. Hensley ML, Miller A, O’Malley DM, et al. Randomized phase III trial of gemcitabine plus docetaxel plus bevacizumab or placebo as first line treatment for metastatic uterine leiomyosarcoma: an NRG Oncology/Gynecologic Oncology Group study. J Clin Oncol. 2015;33:1180-5.
49. Pautier P, Floquet A, Penel N, et al. Randomized multicenter and stratified phase II study of gemcitabine alone vs gemcitabine and docetaxel in patients with metastatic or relapsed leiomyosarcomas: a Federation Nationale des Centres de Lutte Contre le Cancer (FNCLCC) French Sarcoma Group Study (TAXOGEM study). Oncologist. 2012;17:1213-20.
50. Pautier P, Floquet A, Chevreau C, et al. Trabectedin in combination with doxorubicin for first-line treatment of advanced uterine or soft-tissue leiomyosarcoma (LMS-02): a non-randomised, multicentre, phase 2 trial. Lancet Oncol. 2015;16:457-64.
51. Hadoux J, Rey A, Duvillard P, et al. Multimodal treatment with doxorubicin, cisplatin, and ifosfamide for the treatment of advanced or metastatic uterine leiomyosarcoma: a unicentric experience. Int J Gynecol Cancer. 2015;25:296-302.
52. Leitao MM, Hensley ML, Barakat RR, et al. Immunohistochemical expression of estrogen and progesterone receptors and outcomes in patients with newly diagnosed uterine leiomyosarcoma. Gynecol Oncol. 2012;124:558-62.
53. George S, Feng Y, Manola J, et al. Phase 2 trial of aromatase inhibition with letrozole in patients with uterine leiomyosarcomas expressing estrogen and/or progesterone receptors. Cancer. 2014;120:738-43.
54. Signorelli M, Fruscia R, Dell’Anna T, et al. Lymphadenectomy in uterine low-grade endometrial stromal sarcoma: an analysis of 19 cases and a literature review. Int J Gynecol Cancer. 2010;20:1363-6.
55. Feng W, Hua K, Malpica A, et al. Stage I to II WHO-2003 defined low-grade endometrial stromal sarcoma: How much primary therapy is needed and how little is enough? Int J Gynecol Cancer. 2013;23:488-93.
56. Chan JK, Kawar NM, Shin JY, et al. Endometrial stromal sarcoma: a population-based analysis. Br J Cancer. 2008;99:1210-5.
57. Amant F, Floquet A, Friedlander M, et al. Gynecologic Cancer InterGroup (GCIG) consensus review for endometrial stromal sarcoma. Int J Gynecol Cancer. 2014;24(9 suppl 3):S67-S72.
58. Tanz R, Mahfoud T, Bazine A, et al. Endometrial stromal sarcoma: prognostic factors and impact of adjuvant therapy in early stages. Hematol Oncol Stem Cell Ther. 2012;5:31-5.
59. Wade K, Quinn MA, Hammond I, et al. Uterine sarcoma: steroid receptors and response to hormonal therapy. Gynecol Oncol. 1990;39:364-7.
60. Chu MC, Mor G, Lim C, et al. Low-grade endometrial stromal sarcoma: hormonal aspects. Gynecol Oncol. 2003;90:170-6.
61. Thanopoulou E, Aleksic A, Thway K, et al. Hormonal treatments in metastatic endometrial stromal sarcomas: the 10-year experience of the sarcoma unit of Royal Marsden Hospital. Clin Sarcoma Res. 2015;5:8.
62. Mizuno M, Yatabe Y, Nawa A, et al. Long-term medroxyprogesterone acetate therapy for low-grade endometrial stromal sarcoma. Int J Clin Oncol. 2012;17:348-54.
63. Kurihara S, Oda Y, Ohishi Y, et al. Endometrial stromal sarcomas and related high-grade sarcomas: immunohistochemical and molecular genetic study of 31 cases. Am J Surg Pathol. 2008;32:1228-38.
64. Sutton G, Blessing JA, Park R, et al. Ifosfamide treatment of recurrent or metastatic endometrial stromal sarcomas previously unexposed to chemotherapy: a study of the Gynecologic Oncology Group. Obstet Gynecol. 1996;87:747-50.
65. Tanner EJ, Karuna G, Leitao MM, et al. High-grade undifferentiated uterine sarcoma: surgery, treatment, and survival outcomes. Gynecol Oncol. 2012;127:27-31.
66. Lin YC, Kudelka AP, Tresukosol D, et al. Prolonged stabilization of progressive endometrial stromal sarcoma with prolonged oral etoposide therapy. Gynecol Oncol. 1995;58:262-5.
67. Takano T, Niikura H, Ito K, et al. Feasibility study of gemcitabine plus docetaxel in advanced or recurrent uterine leiomyosarcoma in undifferentiated endometrial sarcoma in Japan. Int J Clin Oncol. 2014;19:897-905.
68. Arend R, Bagaria M, Lewin SN, et al. Long-term outcome and natural history of uterine adenosarcomas. Gynecol Oncol. 2010;119:305-8.
69. Bernard B, Clarke BA, Malowany JI, et al. Uterine adenosarcomas: a dual-institution update on staging, prognosis and survival. Gynecol Oncol. 2013;131:634-9.
70. Tanner EJ, Toussaint T, Leitao MM, et al. Management of uterine adenosarcomas with and without sarcomatous overgrowth. Gynecol Oncol. 2013;129:140-4.