Variants Identified, Associated with Second Malignant Neoplasms in Hodgkin’s Lymphoma
Researchers at the University of Chicago and colleagues have identified two variants on chromosome 6q21 that are associated with second malignant neoplasms (SMNs) in survivors of pediatric Hodgkin’s lymphoma. The SMNs are linked to radiation therapy used to treat the pediatric cancer.
Researchers at the University of Chicago and colleagues have identified two variants on chromosome 6q21 that are associated with second malignant neoplasms (SMNs) in survivors of pediatric Hodgkin’s lymphoma. The SMNs are linked to radiation therapy used to treat the pediatric cancer.
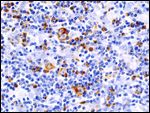
Histopathologic image of Hodgkin's lymphoma. CD30 (Ki-1) immunostain. Lymph node biopsy. It may represent a mixed cellularity type. Source: Wikimedia Commons, user KGH
Dr. Kenan Onel, assistant professor of pediatrics and director of the pediatric familial cancer clinic at the University of Chicago and his colleagues have investigated the variants which are risk loci that are associated both basal and radiation-induced PRDM1 expression, as well as radiation-induced MYC repression. PRDM1 (or BLIMP1) is a zinc-finger transcriptional repressor that is involved in proliferation, differentiation, and apoptosis. Both variants are located in an intergenic region between the ATG5 and the PRDM1 genes.
Cell lines homozygous for both the risk alleles had lower expression of PRDM1 and ionizing radation did not induce expression of the protein; this was untrue of cells that did not harbor the risk alleles. The authors suggest that the gene may be involved in the causation of the radiation-induced SMNs.
In order to identify predisposing risk factors of SMNs in survivors of childhood Hodgkin’s lymphoma, the researchers performed a genome-wide association study (GWAS). SMNs primarily occur in the thyroid, skin, gastrointestinal tract and the female breast. All these organs are involved in the “mediastinal radiation therapy field”. The risk of SMN development is positively associated with the cumulative radiation dose and is inversely correlated with the age at which the original Hodgkin’s lymphoma is treated.
The authors reasoned that narrowing their data collection to those patients that were radiation-treated would enrich the output for genetic variants that may contribute to the risk of SMN development.
18.4% of patients treated for Hodgkin’s lymphoma developed SMNs by 30 years of age. This high prevalence results in SMNs being the second leading cause of mortality in Hogkin’s lymphoma survivors.
PRDM1 normally negatively regulates MYC, a pro-proliferative gene. The authors found that cells homozygous for the risk alleles had significantly more repression of MYC expression after ionizing radiation.
“We found [the variants] by doing a GWAS of radiation-induced SMNs in Hodgkin’s Lymphoma survivors. The fact that MYC is altered in radiation-induced breast cancers and PRDM1 is upstream of MYC may suggest that they mediate their effects on risk directly in the affected tissue (for example, breast) by resulting in differential regulation of PRDM1 targets such as MYC. In cells with the risk haplotype, MYC is less efficiently repressed than in cells with the protective haplotype, which may functionally mimic MYC amplification,” explains Dr. Onel. Dr. Onel and his colleagues are currently investigating whether the effect of these alleles is direct or indirect with follow-up experiments.
The results support a previously unidentified role of PRDM1 as a “radiation-responsive tumor suppressor.” However, it is also possible that an altered immune function or inflammatory response is associated with SMN risk, as other intergenic variants between PRDM1 and ATG5 are associated with autoimmune disease.
“Given that the PRDM1 single nucleotide polymorphisms (SNPs) have been previously associated with non-Hodgkin’s lymphoma and autoimmune disease, an alternative hypothesis might be that they are associated with SMN risk indirectly, that is, by mediating an altered immune response to radiation. Since chronic inflammation is associated with cancer, one might hypothesize that a pro-inflammatory immune response may be also be associated with increased risk for cancer. Since PRDM1 is important in B-lineage development (its alternate name is BLIMP1), it is not unreasonable to assume it may have an important regulatory role in the immune system” elaborated Dr. Onel.
Because children treated with lower-dose radiation therapy for Hodgkin’s lymphoma are still at risk for SMNs, this research will likely be important to understand the causality of SMNs in survivors of childhood Hodgkin’s lymphoma as well as other radiation-treated cancer patients.
Dr. Onel stated that he and his colleages are “investigating the pathways activated by PRDM1 in response to radiation in order to understand how we might modify it to make radiation safer for patients with the risk haplotype, possibly through some sort of radio-protective drug.”
“Our data suggest that individuals with the protective haplotype have a 3% risk of developing a radiation-induced SMN by 30 years following radiation therapy while those with the risk haplotype have a 30% risk. The problem is that while those estimates are striking and our results in the paper indicate a mechanism, they are based on relatively small numbers of patients, and so, the confidence interval is large. Consequently, they are not ready yet to be used clinically. We are working hard to test the association between our SNPs and radiation-induced cancers in other patient sets in order to move our findings to the clinical realm, both for Hodgkin’s lymphoma survivors and for other patients treated with radiation thearpy who may also be at risk for radiation-induced SMNs” said Dr. Onel.