Veliparib Trial Fails to Improve Outcomes in Ovarian Cancer
Adding the PARP inhibitor veliparib to cyclophosphamide did not improve response rates or progression-free survival in ovarian cancer.
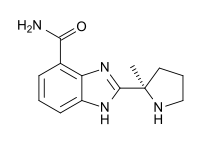
Chemical structure of veliparib
Use of the PARP inhibitor veliparib in combination with oral cyclophosphamide did not result in an improvement in response rate or median progression-free survival compared with treatment with cyclophosphamide alone, according to a phase II study evaluating patients with high-grade serous ovarian cancer, peritoneal, fallopian tube, and BRCA-mutant ovarian cancers.
However, the study did demonstrate that oral cyclophosphamide was well-tolerated among this patient population and was associated with responses and prolonged disease stabilization.
“The relative sensitivity of tumor cells carrying various defects in the homologous recombination (HR) pathway to PARP inhibition is not well characterized, and therefore it is not known whether including patients likely to carry other defects in the HR pathway (high-grade serous ovarian cancer) as well as patients carrying known deleterious mutations in BRCA1 or BRCA2 in a relatively small sample set may have affected the overall outcome of the trial,” Shivaani Kummar, MD, of the National Cancer Institute, and colleagues wrote in Clinical Cancer Research.
“The lack of increased response rate with the addition of veliparib to cyclophosphamide could also be due to the dose of veliparib employed in our study, which was below the 250-400 mg BID doses used in recent trials such as the Gynecologic Oncology Group (GOG) trial of single agent veliparib and others.”
The study included 75 patients who were randomly assigned to cyclophosphamide 50 mg with (n = 38) or without veliparib 60 mg orally (n = 37) in 21-day cycles. Of the 75 patients, 72 were evaluable for response.
There was one complete response reported in each of the treatment arms. Six patients (19.4%) assigned to cyclophosphamide alone had partial response compared with three patients (11.8%) in the combination arm. Four of the patients with responses to cyclophosphamide had BRCA-mutant ovarian cancer, two had high-grade serous ovarian cancer, and one had fallopian tube cancer.
The median progression-free survival was 2.3 months for patients assigned cyclophosphamide alone compared with 2.1 months for combination treatment. Stratification of patients by BRCA status did not reveal any significant improvement in progression-free survival.
The researchers conducted genetic sequence and expression analysis for 211 genes involved in DNA repair; however, none of the genetic alterations were associated with any treatment benefit.
Grade 2/3 leukopenia was the most common adverse events reported among patients in both arms. Two patients assigned to combination treatment reported grade 4 lymphopenia that requiring a dose reduction.