Adding Carfilzomib to Myeloma Treatment Results in ‘Unprecedented’ Boost in PFS
Adding carfilzomib to lenalidomide and dexamethasone resulted in a higher PFS and better overall quality of life for relapsed multiple myeloma patients.
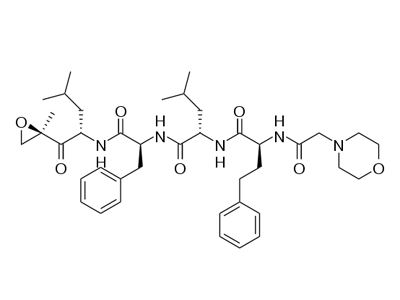
Chemical structure of carfilzomib
Adding carfilzomib (Kyprolis) to the standard doublet therapy of lenalidomide and dexamethasone resulted in a higher progression-free survival (PFS) and better overall quality of life for relapsed multiple myeloma patients. These results of the phase III ASPIRE trial were presented at the 2014 American Society of Hematology (ASH) Annual Meeting, held December 6–9 in San Francisco.
The data were also published in the New England Journal of Medicine.
Speaking at a press conference, presenter A. Keith Stewart, MB, ChB, of the Mayo Clinic in Scottsdale, Arizona, said the median PFS for the triplet combination is “unprecedented in first relapse multiple myeloma.” According to Stewart, the best median PFS achieved in a clinical trial with a similar patient cohort was 19.6 months.
The difference in the median PFS between the two treatment arms was 8.7 months. The median PFS was 26.3 months in the triplet combination arm compared with 17.6 months in the control arm (hazard ratio [HR], 0.69; P < .0001). The median duration of response was 28.6 months and 21.2 months in the experimental and control arms, respectively.
Carfilzomib is a proteasome inhibitor drug administered intravenously. The drug was approved in 2012 by the US Food and Drug Administration for the treatment of multiple myeloma patients who have received at least two prior therapies, including bortezomib.
Objective response rates were also higher with the addition of carfilzomib. In the experimental arm, 87.1% of patients responded to therapy compared with 66.7% of control arm patients (P < .001). “Even more impressively, I think, the complete response rate was more than three times higher for the patients who took three drugs instead of two drugs,” said Stewart at the press conference. The rate of complete responses was 31.8% for the triplet therapy compared with 9.3% for the control regimen (P < .0001). The mean time to response was 1.6 months in the experimental arm and 2.3 months in the control arm.
The ASPIRE trial enrolled 792 patients internationally. Carfilzomib was administered as a 27 mg/m2 dose on days 1, 2, 8, 9, 15, and 16 of a 28-day cycle and discontinued after 18 months. The drug was given as a 20 mg/m2 dose on days 1 and 2 of the first cycle.
The median overall survival has not yet been reached. However, “there is a trend in favor of the triplet, Kyprolis-containing combination,” said Stewart (HR, 0.79; P = .018). The 2-year overall survival rate is trending in favor of the triplet combination: 73.3% compared with 65.0% for the doublet combination.
Adverse event rates were similar in both treatment arms, which is “very encouraging,” said Stewart. The rates of patients who had grade 3 or higher treatment-related adverse events were 83.7% and 80.7% in the experimental and control arms, respectively. A higher percentage of patients discontinued the treatment in the control arm compared with the carfilzomib-containing regimen (17.7% vs 15.3%). According to Stewart, there was no increase in peripheral neuropathy, suggesting that carfilzomib does not cause this adverse event.
The rate of death due to adverse events was the same, 6.9% in both treatment arms. “This is despite that a third drug has been added and despite the fact that the patients on the triple combination stayed on therapy for 88 weeks compared to control arm, which was on therapy for 57 weeks,” said Stewart.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.